|
CONTENTS
THE EVOLUTION OF MEDICAL CARE
IN THE 19th
CENTURY
QUACKS, SURGEONS AND DOCTORS:
Bartholomew Rolls
John Lloyd
William Firth
Arthur Ballie
Robert Jeninges Moody
Peter Richard Dewsbury
Edward Pope
Charles Percy Green Townsend
Richard Nicholson Lipscomb
Edwin Joseph Le Quesne
James Brown
William Ward Anderson
Charles Edward O’Keeffe
Henry Norman Knox
Edward Middleton-Brown
MEDICAL OFFICERS OF HEALTH:
Charles Edward Saunders
William Gruggen
Malcolm Gross
DENTISTRY
――――♦――――
THE EVOLUTION OF MEDICAL CARE IN THE 19th CENTURY
|
 |
|
Bleeding a
patient |
By the end of the 18th Century (and for many years thereafter)
smallpox, typhus and tuberculosis were endemic, and cholera
alarmingly epidemic.
Medical care was a combination of chance and quackery. Treatments were
mainly botanical, although preparations that contained phosphorous
and heavy metals such as mercury, arsenic and iron were also
popular. Local doctors - in this era generally referred to
as ‘surgeons’ - might recommend a ‘change of air’ together with
vomiting and laxatives and/or the old favourites of bleeding or
leeches. Yet a century later medicine administered by
professionally competent practitioners would be available in a form
recognisable to anyone today - hospitals, stethoscopes, antiseptics,
x-rays, etc.
Broadly speaking, three main branches of medicine had evolved with
some overlap between them. ‘Physicians’ (who were rather thin on
the ground, especially in the provinces) advised and prescribed
medications, ‘apothecaries’ compounded and dispensed those remedies,
and ‘surgeons’ performed all physical intervention from bloodletting
to amputation. Of the three, physicians were held in the highest
esteem because they were university trained and held a degree in
medicine. The possession of this degree entitled them to the title
of ‘Doctor of Medicine’ or simply ‘Doctor’.
At this time there was no university training for the physicians’
less eminent brethren, the surgeons, who acquired their knowledge
through serving apprenticeships to experienced surgeons.
Nevertheless surgeons organized themselves into trade guilds, and
although earlier guilds existed, the roots of today’s practice stem
from the formation in 1745 of the Company of Surgeons. In 1800
this company was granted a Royal Charter to become the Royal College
of Surgeons in London, and it became customary for surgeons to
take the examination for Membership of the Royal College of Surgeons
and put MRCS after their name. However, because
qualification did not result in the award of a university degree,
licentiates could not style themselves ‘Doctor’ and so continued to
be addressed as ‘Mr.’, a tradition that continues to the present day
with female surgeons styling themselves ‘Mrs.’, ‘Miss’ or ‘Ms.’ as
appropriate.
Regulation of the medical profession in the U.K. - leading to what
in modern terms we would recognise as ‘general practitioners’ (GPs)
- followed the passing of the Apothecaries Act (1815) described as “An
Act for better regulating the Practice of Apothecaries throughout
England and Wales.”
The Act made it compulsory
for all new entrants to general practice to acquire the Licence of
the Society of Apothecaries (LSA).
It not only introduced compulsory
apprenticeship, but required apprentices to receive instruction in
anatomy, botany, chemistry, materia medica [1] and “physic”
in addition to gaining 6 months’ practical hospital experience.
The process could begin at age 14, but the minimum age for sitting
the LSA examination was 21. [2] Training typically took 7 years to
complete, with those completing the process successfully gaining the
qualification ‘Licentiate of the Society of Apothecaries’ (LSA).
A large majority of general
practitioners, however, having acquired the LSA qualification also
acquired the MRCS, so that the dual qualification MRCS LSA gradually
became that of the general practitioner.
Oddly, just as it became compulsory for generalist medics to gain
the LSA qualification it seems they largely stopped calling
themselves ‘apothecaries’, preferring instead to use the term
‘surgeon,’ while the ‘apothecary’ gradually assumed the
modern term ‘chemist’ or ‘pharmacist.’ But despite the requirements of the 1815 Act, medical training remained
disparate. Thomas Bonner noted that “The training of a
practitioner in Britain in 1830 could vary all the way from
classical university study at Oxford and Cambridge, to a series of
courses in a provincial hospital, to ‘broom-and-apron apprenticeship
in an apothecary’s shop.’” [15]
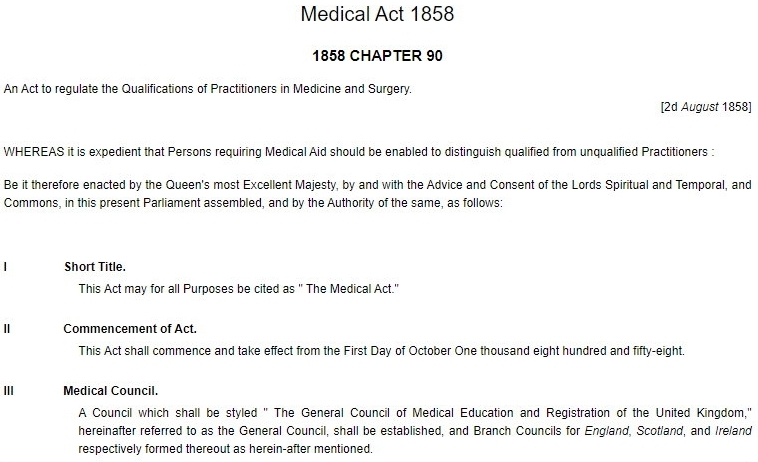
No significant advances were then made until 1858, when the
Medical Act established a recognisable form of healthcare
regulation. The Act’s overall aim was “to regulate the
Qualifications of Practitioners in Medicine and Surgery.” It
established the ‘General Council of Medical Education and
Registration of the United Kingdom’ (‘General Medical Council’
or GMC) as a statutory body and required it to create and publish an annual register of those with specified qualifications who
were entitled to practise medicine or surgery (those in practice
since before 1815 qualified automatically).
[9]
The first official
annual Medical Register showing place of education and qualification
was printed in July 1859. Any person not on the Register (including
anyone struck off) who was practising as a physician, surgeon,
doctor or apothecary was liable to a heavy penalty.
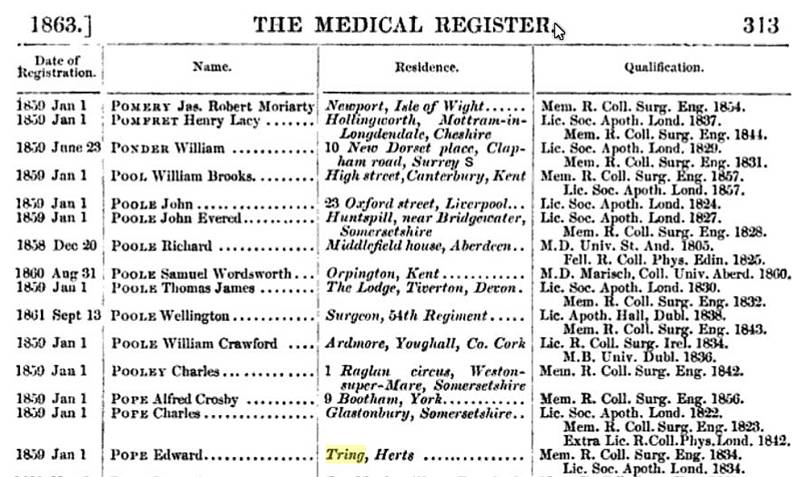
The
Medical Register entry for Edward Pope of Tring listing his
qualifications;
Member of the Royal College of Surgeons England (1834) and
Licentiate of the Society of Apothecaries, London, 1834.
In today’s terms Pope would be considered a general practitioner.
Thereafter medical training became more formal with the
establishment of medical schools, while the number of doctors
increased considerably, from 14,415 physicians and surgeons in
England and Wales in 1861 to 35,650 in 1900. Because the LSA did
not cover surgery, it became the norm at the end of an
apprenticeship for surgeon-apothecaries to take the Royal College of
Surgeon’s membership examination (MRCS) at the same time as the LSA.
So the main qualifications that dominated the profession in the 19th
century became, typically, LSA and MRCS for a generalist (the
precursor of our present day family doctor); and typically MD (a
university graduate in medicine) and FRCS (Fellow of the Royal
College of Surgeons) for the increasing number of hospital based
specialists in medicine or surgery respectively.
――――♦――――
QUACKS, SURGEONS AND DOCTORS
|
 |
|
The Quack. |
Newspapers of the Georgian and Victorian era often contained a
smattering of advertisements for bizarre medications. The quacks
selling these products sometimes colluded with newspaper publishers,
who not only ran the vendors’ advertisements in their pages, but
often - for a cut of the profits - sold the remedies on the
printers’ premises. An example of quackery occurred in December,
1790, when an advertisement appeared in the Northampton Mercury
that commenced as follows:
HYDROPHOBIA:
or, a cure for the bite of a mad dog.
PAUL
NEWENS,
of Wing, in the County of Bucks, is the sole preparer of a medicine
that has never, in any instance, failed to eradicate the dreadful
Malady occasioned by the bite of a mad dog, and which has been
prepared with universal success for these last forty years and
upwards, by the said Paul Newens . . . .
The rabies advertisement - for rabies was the disease in
question - goes on to claim that . . . .
ELIZABETH
KEMPSTER,
servant to Mr. William Stevens, of Marsworth, farmer, had every
appearance of hydrophobia, but on Paul Newen’s medicine being
administered, was in the course of four hours entirely released and
cured.
The advertisement concludes with the names of three individuals able
to testify to the efficacy of this miracle remedy, one of whom was “J.
R. Fawcett, surgeon of Tring.” Fawcett was probably as bogus as
the remedy, for I can find no further mention of him; but bogus or
not, Fawcett is the earliest name connected with medicine in the town
to appear in the press. Today, the promotion and advertising of
medicinal products in the U.K. is governed by advertising laws and
the Human Medicines Regulation 2012, which is enforced by an agency
of the Department of Health and Social Care, the ‘Medicines and
Healthcare products Regulatory Agency’.
――――♦――――
BARTHOLOMEW ROLLS
It is very likely that there were earlier medical practitioners in
Tring - for instance Tring’s burial register records that “Mary the wife of
Jno. Lacy Dr. in Physicke buried March 16th” (1710 or 11) - but
John Lloyd is the first I can trace about whom anything at all is
known. On the 17th April, 1797, it was recorded in the Tring Vestry
Minutes that “The Vestry have agreed to give Mr. Rolls Surgeon
thirty pounds for the year for all cases of Physic and surgery for
the poor.” Some years later a notice appeared in the
London Gazette,
the official public record, to the effect that . . . .
“The partnership lately carried on between Bartholomew Rolls
and John Lloyd
[below], of Tring, in the Country of
Hertford, Surgeons, Apothecaries, and Man-Midwives, is this day
dissolved by mutual consent, as from the 10th April last; and all
accounts relating thereto will be settled by the said John Lloyd,
who will in future carry on the above Professions in Tring
aforesaid, on his own account. Witness our hands this 5th day of May
1815.”
Other than a brief mention in Tring’s Vestry Minutes, no record of
Rolls’ work in Tring appears to have survived. However, an
impression of one aspect of his work – also shared by others
referred to in this paper – comes from his appearance as an
expert witness at a coroner’s hearing where cause of death needed to
be established. This case concerned Sidney Sadler, a printer, who died following a
pugilistic contest in the Islington area of
London. Sadler, reputed to be a quarrelsome individual,
had challenged one John Watts to fight, a challenge that Watts accepted.
Having fought a dozen rounds, Sadler received two blows, one being
to the throat, after which he fell to the ground. Having by then lasted half an
hour, the contest finished. Later that evening
Bartholomew Rolls was called to attend to Sadler, whom he found
sitting in a chair in a public house “quite dead”. Rolls then . . .
.
“. . . . opened a vein in each arm, and then the temporal artery.
On opening the body, he found the marks of a blow (not severe) on
the left side; on opening the head, he found that one of the
arteries of the brain was ruptured, and a great effusion of blood,
which he considered produced apoplexy.
Coroner. ― Did that rupture proceed from a blow?
Witness
[Rolls]. ― It is impossible to say ― it might have proceeded from a blow; or
passion would have produced the same effect.
Juror. ― Would the blows on the jaw have produced the same effect?
Witness
[Rolls]. ― No, certainly not; the body was in a very healthy state, and
they having fought on grass I am inclined to think his death was
caused by apoplexy . . . .
. . . . The Jury then retired to view the body, and, after some
discussion, returned the following verdict: ― ‘The deceased died of
apoplexy, caused by irritation of mind in fighting.’”
Morning Advertiser
23rd October, 1823
On the 8th July, 1826, it was announced in the deaths column of the
Northampton Mercury . . . .
“Lately, in the 58th years of his age (at the house of his son in
law, Mr. Cheney, Aylesbury), Bartholomew Rolls, Esq. of
Pentonville, Middlesex, formerly surgeon of Tring Herts. ― He was
greatly respected in life, and his death is much lamented by his
family and friends.”
――――♦――――
JOHN LLOYD

The grave of John Lloyd,
surgeon, Tring Parish Church.
At the front of Tring Parish Church on its western side stands a
weathered gravestone that bears the barely legible inscription . . .
.
“Sacred to the Memory of John Lloyd Surgeon of this Town who
died November 12th 1825 aged 39 years leaving a Widow and six
Children to lament his irreparable loss.
This stone was erected by a few friends to whom his professional
Talent and private Virtues had justly endeared him.”
Lloyd’s headstone, having been erected “by a few friends”,
gives a hint that he might have been living in straightened
circumstances at the time of his death, a suspicion strengthened by
an entry in the London Gazette (22nd February, 1817)
requiring Lloyd - “Surgeon, Apothecary, Dealer and Chapman” -
to appear at the Guildhall, London, there to make a full disclosure
of his estate and effects. The notice also invited Lloyd’s
creditors to come prepared to prove their debts, for he had been
declared a bankrupt - that said, the Gazette announced his
discharge a few weeks later. What little is known about Lloyd was
that he had been in partnership with Bartholomew Rolls at Tring,
a partnership that was dissolved in 1815, while his death notice
refers to him being “a very eminent surgeon, formerly a partner in the firm
of Messrs. Williams and Lloyd at Brecon.”
In the case of Lloyd, Williams and Bartholomew Rolls it’s difficult
to know exactly what training and skill their use of the description
“surgeon” implies. One can be sure that surgery, both then
and now, involved cutting into the body, but there the comparison
with today’s practitioners ends. What knowledge surgeons of the
time had of surgical procedures will have been acquired through
apprenticeship to a surgeon, who in their turn had also acquired
their knowledge through on-the-job-training. In this context it is
interesting to note that Lloyd and his erstwhile partner Williams
had themselves advertised for such an apprentice . . . .
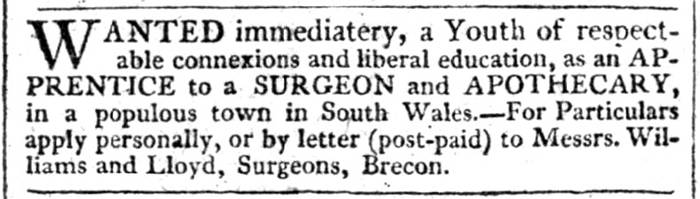
Hereford Journal,
25th January 1809.
The 1823 edition of Pigot’s directory for Tring lists two surgeons,
William Firth and John Lloyd under the heading ‘Professional’, while
the 1825 edition introduces the heading ‘Surgeons’ under which are
listed two partnerships, Firth & Ballie, and Lloyd & Dewsbury.
Although not shown as being in partnership it appears that on at
least one occasion Firth and Lloyd worked together:
“The last week has added two cases to the many incidents which have
occurred on the Grand Junction Canal
[later renamed the Grand Union Canal]. A woman and her daughter, on
their way to Uxbridge in a boat, were, in consequence of the boat
striking violently against the sill of a lock, thrown down with
violence, and a quantity of nails in bags falling upon them, they
were severely bruised, and the woman’s wrist so dreadfully
dislocated, that amputation seemed indispensable. Mr Firth,
surgeon of Tring, however, with a laudable desire to preserve the
limb, called in the assistance of Mr. Lloyd, and the
dislocation was reduced, and hopes are entertained of the poor woman
doing well. The girl, beside suffering very severe bruises, was
very near losing the sight of one of her eyes, a nail having
penetrated just under it.”
Evening Mail,
1st November 1824
――――♦――――
WILLIAM FIRTH
I have been unable to discover anything about William Firth, other than his
entries as a surgeon in the 1823 and 1825 editions of Pigot’s
Directory for Tring.
The Morning Herald
contains a report of Firth attending the victim of a road traffic
accident . . . .
“On Saturday evening last, about nine o’clock, a son of Mr. Walter,
of Wilstone, accompanied by a labouring man of the name of Archer,
were proceeding from Tring towards Wilstone in a taxed cart. The
horse took fright and ran away to the top of the bridge, crossing
the Grand Junction Canal at Little Tring, when the back tree of the
harness gave way, and they were both precipitated out of the cart
with great violence down a steep hill. Young Walter was thrown
against some railings, and fortunately escaped with only a bruise in
the side, from the effect of which he is recovering; but Archer
pitched on his head upon the ground, and the wheel of the vehicle
went over his leg; his scalp was cut open in a dreadful manner, and
he was taken up senseless, and apparently dead, the wound bleeding
profusely; however, he revived, and by the prompt assistance of
Mr. Firth, a surgeon of Tring, was sufficiently restored to be
conveyed home, where he now lies, suffering dreadfully from the
accident, but great hopes are entertained of his recovery.”
Morning Herald, 25th August, 1825
I was unable to locate anything further about this accident. As for
Firth and his partner Ballie, neither appear
in the 1839 edition of Pigot, the next edition available to
me.
――――♦――――
ROBERT JENINGES MOODY
In Pigot’s directory for 1839,
under SURGEONS
appears one
“Moody Robt. Jeninges” whose practice was at Frogmore House (once located
in Frogmore Street, Tring, long-since demolished). Moody appears to have been
born in Great Missenden on the 26th August 1807, married Charlotte
née Cutler, and died at Tring in January 1842. The National
Archives holds the will of one Robert Jeninges Moody,
“Druggist of Great Missenden, Buckinghamshire,” but dated 1st June 1842.
Whether these references relate to the same person I cannot say,
but I can find no other information relating to a surgeon of that
name practicing in Tring.
――――♦――――
ARTHUR BALLIE M.R.C.S.
In June, 1830, Tring surgeon Arthur Ballie attended Samuel Budd, the
victim of a road accident possibly caused by his carthorse shying.
Budd later died of his injuries. In the absence of any
method for assessing the extent of
the victim’s internal injuries, the press
report of the inquest illustrates both the surgeon’s speculative
diagnosis and the lack of any effective
treatment in his repertoire:
“An inquest on the body
of Samuel Budd, was held on Wednesday, 23rd June
[1830], before F.
J. Osbaldeston Esq., at the Rose and Crown Inn, Tring . . . . Job
Nutkins said he works for Mr. Stevens, Tring Grove. Knew deceased;
saw him alive on Monday morning, about seven o’clock, sitting up on
the road. Saw a cart lying on the road; the cart had been turned
over on the near wheel; the horse was about six yards from the cart;
the shafts of the cart were broken . . . . deceased was about five
yards behind the cart . . . . spoke to deceased, but he did not
answer; there was blood on his temples, though not much . . . .
“Mr.
Arthur Baillie, surgeon, examined
[by the coroner], said he was sent for about seven on Monday morning to see
deceased who was at his own cottage in bed. Deceased
complained of pain in his chest, and stomach; his breathing was very
laborious. Witness
[Baillie] found a great depression in the lower part of the sternum; and a
fracture of the large rib on the left side. There were also
slight marks on the left side of the head; but not sufficient to
produce death. Witness was of the opinion that the concussion
of the chest produced death. Deceased’s extremities were cold.
Witness gave him some brandy to stimulate him and subsequently bled
him, but he gradually got worse, and died about nine yesterday
morning. Verdict accidental death.”
Bucks Gazette,
26th June 1830
Ballie appears again in the coroner’s court in September 1831 in a
case reported in the Bucks Gazette that illustrates how
helpless the surgeons of the time were at treating serious injury.
The circumstances of the death of Thomas Lovett are summed up in the
verdict of the coroner’s jury:
“The jury returned a verdict in substance as follows: ‘That the said
Thomas Lovett, on the 1st Sept., 1831, received a mortal wound of
the depth of four inches, and of the breadth of one inch, in his
left thigh, by a loaded gun, which he had been carrying when in the
act of sporting, having gone off accidentally, and the contents
thereof having penetrated his thigh, of which wound the said Thomas
Lovett on the said 1st Sept. died.’ The verdict was accompanied by
this observation - ‘But the jury are of the opinion that too large
quantities of opium were injudiciously administered to the said
Thomas Lovett.’”
Bucks Gazette 10th September, 1831
Following the gunshot injury, Lovett was taken to his house and
Ballie was sent for. Two other surgeons, Ayckburn of Wendover and
Rumsey of Chesham, arrived later. Lovett, who
complained of great pain, had received a large lacerated wound on
the back of the thigh. Ballie stated to the coroner that:
“On
introducing my fingers into the wound, I found it plugged up with
coagulated blood, and the thigh bone was shattered, the upper
portion of which protruded through the wound . . . . the patient
complained of extreme pain; and as soon as I could procure pillows,
I placed the limb in a more comfortable position. . . . The deceased
repeated his wish to have something administered to him to ease his
pain: I sent home for a draught, directing thirty drops of tincture
of opium to be used in syrup and camphor mixture; also for a small
phial of tincture of opium and compound spirits of ammonia.”
Before the opium arrived, Ballie treated the patient’s thirst by
administering “to the patient some tea from the spout of a teapot.”
In consultation with the other surgeons it was agreed that
amputation would be necessary if the patient rallied. One of their
number, Mr. Ayckburn of Wendover, administered pain relief in the
form of opium to a total dose of 8 grains, [16] but
Lovett grew increasingly weak and died. Ballie informed the coroner
that:
“I am of the opinion that an excess of opium was given
according to the circumstances of the case, and that the sudden
termination of the case by the death of the patient was attributable
to the opium acting upon the nervous system of the patient, who had
not rallied from the first shock . . . death was accelerated by the
treatment. The patient did not rally sufficiently during the day to
warrant amputation.”
Considering the primitive surgical techniques
of the time, I think it highly doubtful that amputation would have
produced a beneficial outcome.
During the hearing Ayckburn informed the coroner that he was
qualified by experience rather than examination - “I am not a
member of the College of Surgeons, nor a Licentiate from the
Apothecary’s Company; I have been in practice 25 years.” Ballie,
on the other hand, was at least partly qualified, being a member of
the Royal College of Surgeons.
――――♦――――
PETER RICHARD DEWSBURY Sh, L.S.A.
Little is known about Dewsbury the man. Born at Chester, the
1851 Census locates him and his family (wife, daughter, medical
assistant, cook, groom and housemaid) living on Tring High Street.
He was then 48 years of age so his death
in 1857
(cause unknown)
came at the comparatively early age of 54. In the Census Dewsbury
uses the then fairly novel term ‘General Practitioner’ to describe
his occupation, and gives his qualifications as Sh (unknown) and LSA
(Licentiate of the Society of Apothecaries).
Dewsbury appears in the press periodically, generally as an expert
witness in the cases that required a medical opinion on cause of death. Such was the case in a pugilistic
contest that took place at Wigginton in December 1827. The
rules of such contests allowed for a broad range of fighting
including holds and throws of the opponent. A round ended with
one contestant being downed by a punch or
throw, whereupon he was given 30 seconds to rest and eight
additional seconds to return to the centre of the ring to continue. Consequently,
a fight did not end after a limited number of rounds, but when one participant
was unable to continue.
Such a contest between James Kindell and John Olliffe resulted in
the death of Olliffe.
Kindell eventually stood trial at the Hertford Assizes accused of
“feloniously killing and slaying John Olliffe, on the 11th of
September, at Wigginton.”:
“Harding Dell
[a labourer]
stated, that, on the day in question,
there was a feast on Wigginton-green, at which he, the prisoner, the
deceased, and about 100 other persons were present. In the course
of the day, the prisoner and the deceased talked about fighting.
The deceased stripped first and on being advised not to fight, said,
‘he must, for he was put upon,’ and then called out to the prisoner,
‘Come, Jemmy, I’m ready for you.’ They then fought: it was a fair
stand-up fight, and the prisoner had the worst of it for several
rounds. At length he struck the deceased a severe blow on the left
side, which threw him: but they fought three or four rounds
afterwards, when the deceased gave in, and died in half an hour.
The body was taken to the house of the sister of the deceased, and a
surgeon sent for . . . .
. . . . Mr. Dewsbury a surgeon at Tring saw the body about eight
o’clock on the evening of Tuesday; found him dead; had the clothes
stripped off the body; on the left side of the chest, in the
abdomen, discovered a considerable bruise, and some slight bruises
on the left side of the neck, a fracture, or incised wound; did not
attempt to bleed him; attended on the morning of the inquest, and
opened the body; on opening the body found a considerable quantity
of coagulated blood in the cavities of the abdomen; on removing that
fluid discovered a rupture of the spleen, which was quite sufficient
to account for the man’s death; believes that violent contraction of
the muscles of the spleen might have produced the rupture, but
believes this was caused by a violent blow, which in his opinion was
the case.”
And then took place a curious turn of
events.
Dewsbury was proceeding to state that he had examined the
body of “a man” on the day in question
. . . .
“. . . . when,
on being asked whether he knew the name and person of the deceased,
he replied in the negative; and no witness being forthcoming to
prove that the body examined by Mr. Dewsbury was the body of the
deceased, John Olliffe, the Learned Judge interposed, and said that
a verdict of acquittal must be taken, as there was no evidence of
the identity of the body, or, consequently, of the cause of the
death of the deceased.
The prisoner was accordingly acquitted.”
Derby Mercury, 12th December, 1827
When the London & Birmingham Railway opened in September 1838,
several publishers saw an opportunity to cash in on this novel form
of transport by publishing guide books to the line. As passengers
progressed along it, with the help of their travel guide they could compare the view from the
carriage window
with the writer’s description of the countryside and
the towns through which the line passed (or, in the case of Tring,
passed at some considerable distance).
Osborne’s Guide (1838) gives a good potted account of Tring
at the time including a reference to its Silk Mill, most of which
remains in Brook Street. The “fish pool”, which at the
time was much larger than today, was originally used as a pond from
which water was drawn to power the mill’s machinery, but by the time
of
Osborne water power had been replaced by a steam engine. It
is interesting to note the writer’s observations on the health risk
posed by the pond:
“By the side of the mill is the temporary residence of the
proprietor, with a conservatory, and an extensive fish pool, the
rather stagnant nature of which must give rise to much of pernicious
effluvia
[an unpleasant or
harmful odour or discharge]; and considering that Tring is seldom or never without ague
[fever],
and as the malaria
[3] is generally found to result from pools of this character,
several of which are in the vicinity, it is to be hoped that, ere
long, the proprietors of these sources of pestilence will evince
sufficient morality and intelligence to compel the removal of a
nuisance so highly dangerous to all the neighbourhood; actually
fatal to some, and deeply injurious to the lives and happiness of
many innocent people.”
Osborne goes on to describe the effects of the “pernicious
effluvia” on the mill workers:
“In the mill there are almost always persons whose haggard looks
evince their having lately been afflicted with this terrible
disease, evidently consequential to placing employed in a building
through which there must, despite all precaution, be continually
circulating a portion of the vapour from the pool beneath; the adult
patients look bad enough; but the sight of the little children who
have lately suffered, with their wretched countenances, death-like
colour, and tottering frames, cannot but make the heart of any
humane person burn with the keenest anguish.”
And it is here, at the Silk Mill, that we again encounter Mr.
Dewsbury, surgeon of Tring:
“The proprietors of the mill pay Mr. Dewsbury, Surgeon, of
Tring, £20 a year for inspecting the persons employed in the mill,
to insure cleanliness and freedom from disease: after this evidence,
we must not attribute the presence of the injurious marsh to a want
of feeling in the proprietors, but rather to a want of information
on the subject.”
Whether Mr. Dewsbury delivered any real value for his fee is
doubtful. From what Osborne says, those suffering the “ague”
exhibited symptoms that were plainly evident, while it is
unlikely that Dewsbury had any effective remedy at his
disposal to combat the condition. The affliction, whatever it was, was not airborne as was
thought at the time, but was more likely to have been contracted
from well water polluted by waterborne bacteria
stemming from inadequate (or non-existent) sanitation. Tring had to
wait until the 1870s to receive a mains supply of clean drinking
water, and even then many would not pay the water company’s fee for connection
to it.
Another case that involved the newly opened London and Birmingham
Railway occurred in October 1838 and caused something of a scandal. The
President of the
Royal College of Physicians, Sir Henry
Halford, had invited a friend, George Lockley, to spend some time
with him at his home in the country. Shortly before arriving at
Tring Station on their journey north, Lockley suffered an “apoplectic fit” (a
stoke). The report in the Morning Chronicle continues:
“The train having arrived, the officers were beckoned to one of the
carriages, and thus accosted by a venerable-looking personage
within: ― ‘Officer, here is a very respectable gentleman,
extremely ill. Do take great care of him, and send off immediately
for medical advice’ . . . . Did this friend even get out of
the carriage? He did not, but, frightful to relate, actually flew
off with the train, leaving his senseless and speechless friend in
the open road, and supported in a chair, placed on the cold wet
clay, by the hands of the official strangers! Mr. Lockley was
treated with marked humanity and attention by the officers of the
railway who conduct the business of that station . . . .”
What then transpired varies
between newspaper reports, but according the The Atlas:
“In about an hour Mr. Dewsbury arrived, and bled Mr. Lockley,
who was removed to the town that evening and expired on the 20th
ult. This is Sir Henry’s own statement, called for by the indignant
feelings of the profession at his having abandoned his friend and
companion, and not attended to him, and applied himself the
resources of his art.”
In response to this charge of neglect, Sir Henry claimed that the
rules of the College of Physicians prohibited from bleeding
(bloodletting), a job that called for a surgeon; as a physician,
Halford could only prescribe. Would bloodletting have helped
Mr. Lockley? Bloodletting was the withdrawal of blood from a
patient to prevent or cure illness and disease, or so it was
believed based on ancient theory. But in the days when doctors
had little in the way of effective treatment there was a need to be
seen to be doing something to treat the patient. Even if there was
no proven medical benefit to be derived from the procedure, its
placebo effect should not be overlooked. Since the modern era of
‘evidence-based’ medicine, the practice of bloodletting has been
consigned to the dustbin of discarded treatments. As for Sir Henry,
the scandal surrounding Lockley’s death did him no lasting damage
professionally, for he continued to serve as President of the Royal
College of Physicians until his death in 1844.
――――♦――――
EDWARD POPE M.R.C.S., L.S.A.
In the graveyard extension to the north of the parish church is the
grave of Edward Pope M.R.C.S., L.S.A., “SURGEON IN THE TOWN
FOR SIXTY YEARS”. He must have been held in considerable esteem by the community, for
inside the church is a memorial plaque.
|
 |
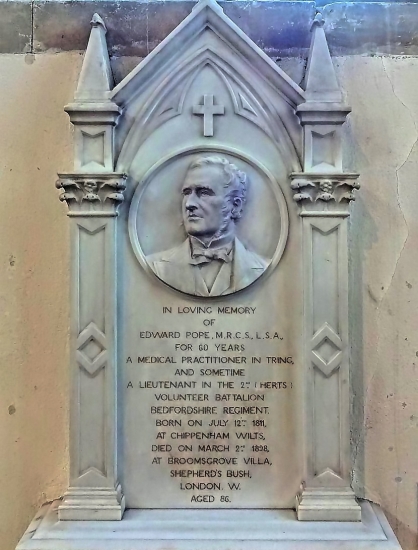 |
|
The Pope
family grave, Tring Parish Church. |
Memorial
plaque to Edward Pope, Tring Parish Church. |
Edward Pope (1811-1898) was born at Frome, Somerset. On leaving
school he was apprenticed to his uncle, Dr. Roberts, of Burnham,
Bucks. He studied at Guy’s, St. Thomas’s, and Webb-street,
qualifying as M.R.C.S. and L.S.A. in 1834. Pope settled in medical
practice in Tring in 1837 in succession to the late Mr. Firth, and
married in the following year. Sadly, death was a frequent visitor
to the Pope household, claiming his wife Catherine in 1875, two
daughters and two sons, all in their childhood or infancy. His son,
Dr. Harry Campbell Pope survived him (d. 2nd January, 1906).
During his career, Edward Pope’s name frequently appears in the
local press, generally in connection with hearings before the
coroner when cause of death needed to be established, but
occasionally a report crops up that is out of the ordinary.
The first took place in Aylesbury in February 1847, when an
event took place that was to have an extraordinary impact on surgical
procedures
carried out in the locality. [4] This from the Bucks Herald:
“On Tuesday last the marvellous effects of the inhalation of the
etheric vapour were developed in three extraordinary cases: — the
amputation a leg, — the removal of a tumour from the shoulder,— and
the extraction of a finger nail, and subsequent application of
strong nitric acid as a caustic. The operations were in each case
most successfully performed, and without the slightest sense of
pain, in the presence of a large number of gentlemen, both of the
profession
[including Edward Pope] and of those
interested in witnessing the wonderful effects of ether, in the
amelioration of human suffering in surgical operations.”
In an age when the serious fracture of a limb usually resulted in
amputation, and with no pain-relief available, lightning-quick
surgery shortened the almost unimaginably horrific trauma of the
amputation. The screaming patient was typically held down on a
wooden bench by “dressers”, who would also assist with ligatures,
knives and dressings. Although not realised at the time,
lightning-quick operations also minimised the exposure of tissue to
infection.
In the case witnessed by Pope, the patient had sustained injury by slipping on a
frosty surface, in consequence of which he . . . .
“. . . . sustained a compound fracture of both bones of the leg. He
was conveyed to the Bucks Infirmary and for some time his life was
in danger from severe erysipelas taking place, and abscesses forming
throughout the upper part of the leg and thigh, precluded any
immediate operation. A further delay was subsequently permitted
with the view of saving as much of the limb as possible, but at
length it was found necessary that amputation should take place . .
. .Shortly after twelve o’clock the patient was brought into the
operating roam, and being placed on the operating table, the
administration of the ethereal vapour was then conducted by Mr.
Robert Ceely . . . . As it was intended to prolong the influence,
the ether was administered gradually, and so as to cause not the
slightest inconvenience to the patient. The full effect was visible
in five minutes, when the patient, being in a perfect state of
insensibility and muscular relaxation, the operation of removing the
limb was commenced by Mr. James H. Ceely, and in one minute and a
half the limb was separated, during which time not the slightest
sensibility or motion was apparent. The securing of more more
vessels than usual, and the final dressing of the stump, farther
occupied nine minutes and a half, the whole operation thus being
performed in 11 minutes.”
Bucks Herald 27th February, 1847
There is no further mention of George Kean in the following weeks’
papers, perhaps an indication that he did not succumb to
infection that in the days before antiseptic surgery claimed the lives of
many who had undergone surgical procedures.
Another unusual event attended by Pope occurred in January 1853. It
concerned clairvoyance, or the ability to gain information about an
object, person, location, or physical event through information
sensed with the mind. And here we meet another Tring
personality,
Gerald Massey, a self taught poet whose writing
attracted considerable attention during the mid-19th century.
Money was for ever short in the Massey household and to help balance
the books the poet would hold public exhibitions to exploit his wife’s talents as a noted clairvoyant. At one such exhibition
held at
the Commercial Hall in Tring, Rosina Massey commenced by reading from any
and every book or paper passed to her from the audience, but with her
eyes effectively covered. In order to prevent collusion or
deception, the audience had been asked to provide their own papers
for Rosina to read. She was then placed by Massey into a “mesmeric
sleep” (i.e. placed under hypnosis) and although papers in some
very small type were handed to her, according to the Bucks
Advertiser (21st January 1853) in almost all instances she read
with her eyes covered to the perfect satisfaction and astonishment
of those present.
Edward Pope, who was in the audience, subsequently wrote to
the Editor of the Bucks Advertiser proclaiming Mrs Massey to
be a fraud and concluding with the pertinent question “Why
accept a shilling or eighteen pence for exhibiting manifestations of
a power which, skilfully applied, would make them [the Masseys]
rich beyond the dream of avarice?”, to which one of paper’s
readers replied [to Pope] “Why, Sir, you mesmerise upon a large
scale, and then find fault with a poor soul that only trades now and
then for a crust.” There was probably truth on both sides of
that argument.
Hydrophobia – or rabies, to use its common name –
was a real threat to
life at a time before this dread disease was brought under control. Pope must have known
the inevitable outcome of rabies, for there was no vaccine at the
time with which to fight it [5]:
“DEATH
FROM
HYDROPHOBIA
AT
WIGGINTON.—
It will be remembered that about two months ago a dog supposed to he
rabid was running about in the neighbourhood of Tring for some
considerable time, and creating much alarm, until it was at last
shot by Mr. E. C. Knight of Tring. Unfortunately, however, the dog
was not killed until several other dogs had been bitten, and two or
three persons also. One of the latter was a boy named Richard
Turney, aged ten, living at Wigginton, who took the dog up in his
arm and fondled it, when it bit him under his chin. Hearing
afterwards that the dog was supposed to be rabid the day after he
was bitten he went to Mr. Pope, surgeon of Tring, who
cauterised the wound.
On Friday week the lad‘s father applied to Mr. Pope with respect to
his son, who was unwell. Mr. Pope went at once and visited the boy,
who, in his opinion, showed symptoms of hydrophobia. He sent him
some medicine, saw him again the next morning, and advised his
removal at once to the West Herts. Infirmary. This advice was acted
upon, but the poor led gradually got worse, and died there on Sunday
night.”
Bucks Herald
27th October, 1877
In addition to his role as a general practitioner, Pope also held
public appointments as ‘Certifying Surgeon of Factories’, [6]
‘Medical Officer for the Tring District of the Berkhamsted Union’,
and ‘Medical Officer for the Aston Clinton District of the Aylesbury
Union.’ [7]
Sanitation at the time was poor due principally to
the lack of safe sewage disposal. Thus, in the absence
of a mains supply of clean drinking water, water drawn from wells and from
brooks was often polluted with faecal matter, which gave rise to the
spread of waterborne diseases such as dysentery, typhoid and cholera. Two reports from 1875
illustrate Pope’s role in combating the problem.
In the first, the tenants of a row of cottages at Aston Clinton were
summoned under the Sanitary Act (1866) to show cause why a well, the
water in which was so polluted as to be injurious to health, should
not be stopped up. The Inspector for the Rural Sanitary Authority
produced for the magistrates a sketch of the premises and pointed out the
different drains, cesspools, &c., all of which were unsealed. As a result
they drained into the well, thus polluting the
water. At the hearing . . . .
“. . . . Dr. Pope of Tring, medical officer, said — I know this
property at Aston Clinton. I have examined the water of the well,
which contains a large amount of organic matter and chloride, which
can only come into it from sewage. The water would be injurious to
health, if drunk, and at some seasons, when low, it is not even fit
for other domestic purposes.
. . . . In reply to the Bench, the Inspector for the Rural Sanitary
Authority said complaints had been made also of the pollution of the
brook water by ducks and cattle . . . .
Dr. Pope suggested the making of a tank for the brook water, at a
point a little higher up than the cottages. He accounted for the
contamination of the well by the overflowing of the cesspools from
heavy rains, and possibly also to the inhabitants themselves
throwing slops into it. He had a sample of the water analysed some
time ago by Dr. Saunders of London, one of the analysts of the
Metropolitan Sanitary Authorities, and he told him it was worse than
that of the Thames at London Bridge.”
Bucks Herald 8th May 1875
Some further remarks were made by the magistrates as to the advisability
of having a fresh well sunk, in reply to which one of defendant said
that their wives were too lazy to draw the water if a well was sunk,
preferring instead to go to the brook which is nearer (referring to
a brook running in front of the houses). In conclusion the Bench
ordered the well to be stopped up for six months, but made no order
regarding the brook. How public health benefitted from this ruling
in the longer term isn’t clear.
The second case also involves cottages at Aston Clinton, this time
with unhealthy arrangements for drainage and the removal of human
waste:
“SANITARY
SUMMONS.—George
Keene was summoned by the Sanitary Authority of the Aylesbury Union
[7] for not complying with a notice given him to repair the drains
of some houses at Aston Clinton, of which he is the owner. Mr.
Newman said he was the inspector of nuisances for Aston Clinton, and
produced authority to take proceedings by minute of the Sanitary
Authority of the Union. He further produced plans of the property,
showing the state of the drains, and also a copy of the notice
served upon the defendant. He said the defendant refused to make
the alterations required, saying that they would do very well. He
was the owner of ten cottages, in one of which he lived. The drains
were in a very bad state.
Mr. Edward Pope, surgeon of Tring, deposed that he had
inspected the drains referred to on Tuesday last. The surface drain
behind the cottages was broken. The drain was made of common
unglazed pipes. The cesspool was open and uncovered, and it ought
to be covered and cemented. The drains were likely to render the
air of the cottages foul, and in his opinion they were in a state
injurious to health.
The defendant did not appear, and the Bench made an order for the
repair of the drains to he carried out within fourteen days.”
Bucks Herald 17th July 1875
In 1899, in the Akeman Street area of Tring, sewage leeching into
unsealed wells from which drinking water was drawn resulted in a
typhoid outbreak that infected 105 people, taking the lives of nine
of them.
――――♦――――
CHARLES
PERCY GREEN TOWNSEND
Under “Surgeons”, the Tring entry in the Hertfordshire Almanac
for 1884 lists “Messrs Pope and Townsend.” Reports of
coroners’ hearings identify Pope’s partner as Charles Townsend, who
qualified at Birmingham in 1875 and appears to have practiced
at Tring between 1881
and 1885, when his partnership with Pope was dissolved. Nothing else is known about him.
Townsend’s name appears in the press in connection with the suicide of Thomas Fowler, a labourer
aged 60 years, who lived at Buckland. His wife awoke during
the night to find that he had cut his throat. The newspaper report went on to
say that . . . .
“Mr. Charles Townsend, surgeon, Tring, said he had attended the deceased for
about six months. He was suffering from a very painful disease.
Witness was sent for early on the morning of the 3rd May, to see the
deceased, and found him with his throat cut. The wound was
deep, but no large artery was severed. The windpipe was
severed entirely. Witness sewed up the wound and dressed it,
and the deceased became convalescent so far as the actual wound was
concerned . . . . The jury returned a verdict to the effect that
‘The deceased died from exhaustion and shock to the system, caused
by the wound which he inflicted upon himself on the 3rd May, he
being at the time of unsound mind.’”
Bucks Herald 4th June, 1881
――――♦――――
RICHARD NICHOLSON LIPSCOMB M.R.C.S. Eng (1855) L.S.A. London (1856)
Most of the personal information available on Richard Lipscomb comes
from an obituary:
“Richard Nicholson Lipscomb was a son of Dr. Lipscomb of St. Albans,
and a grandson of the Rev. Dr. Nicholson, rector of its Abbey
Church. In 1857 he purchased the medical practice of Mr. Dewsbury.
He occupied as his house and surgery premises in the High-street,
since pulled down and now forming part of the Tring Park Estate
office, and here his three children were born. Mr. Lipscomb was
never very strong and usually drove in summer in a victoria and in
winter in his brougham,
[8] while his
professional rival, Mr. Pope, who, although older was much hardier,
either rode or drove in an open gig, and their courteous but
somewhat distant salutations as they met on their daily rounds had
an old-world flavour somewhat reminiscent of Anthony Trollop’s
Barsetshire. In the year 1883, being then not much over 50 years
old, Mr. Lipscomb retired from practice, and went to live at Hove,
where he has resided ever since. For the last few years he was more
or less of an invalid, and a fall down a steep flight of stairs was
the immediate cause of his death. Mrs. Lipcomb predeceased her
husband by some years, as did also his eldest son, but he leaves one
son and one daughter to mourn their loss.”
Bucks Herald, 3rd January, 1914
Lipscomb trained at Guys and the Middlesex Hospital, later becoming
House Surgeon, Acting Resident Medical Officer, and Medical and
Surgical Registrar before coming to Tring (c.1860).
In common with the town’s other medical practitioners,
Lipscomb was occasionally called upon to give evidence at coroner’s
inquests, such as in the case of
William Allen, a farm labourer, who died while gathering in the hay on a farm
at Drayton Beauchamp.
The hay was being loaded onto a cart to be
carried to the rickyard and Allen was standing on top of the pile.
Another labourer who was picking up the rakings heard the sound of
someone falling, and on going to investigate found Allen lying face
downwards
on the far side of the cart
with his arms under him . . .
.
“He was insensible and did not speak, nor did he call out as he
fell, or give any warning that he was likely to do so. He was quite
sober. He had complained once or twice during the day of feeling
unwell. It was very hot working in the fields. Witness did not
think he
[Allen]
lived two minutes after he found him on the ground. The horse was
standing perfectly still at the time. . . .
Mr. Lipscomb, surgeon of Tring, said he had frequently attended the
deceased for asthma, but not lately. He saw him yesterday; he was
then quite dead. There was a contusion on the fore-part of the
head, probably caused by a blow or fall. His skull was not
fractured. His impression was that there was a rupture of the
spinal chord at the back of the neck, which would most likely cause
immediate death. He could not detect any other injuries about the
body. He thought it very likely that the deceased might have taken
giddy, which caused him to fall off the load of hay. Asthma was
frequently connected with disease of the heart.
The jury returned a verdict of ‘Accidental death.’”
Bucks
Herald of 12th July, 1873
Smallpox was one of the biggest viral killers of the 19th century and
Lipscomb played his part in combating the disease with the vaccine
at his disposal.
In 1796, physician Edward Jenner discovered that people who had been
casually infected with cowpox appeared to become immune to smallpox.
However, cowpox was rare and before the commercial manufacture of
vaccine many years later the supply of vaccine depended on its
propagation from human to human – if the vaccine “took” on a child’s
arm, then nine or ten days later a pustule would form that was then
pricked to provide fresh vaccine. Children of the poor were
immunised at no charge and, on returning to clinics for “inspection”,
were put “arm-to-arm” with the next batch of children. But
at a time when the risk of transmitting infection such as syphilis was
little understood, arm-to-arm vaccination was dangerous.
With the onset of the COVID-19 pandemic, anti-vaxxers – people
wholly opposed to vaccinations
– were again in the news, this time with regard to COVID-19
vaccination. But the anti-vaccination movement is not new; it is as
old as vaccines themselves. Widespread vaccination of children
began in the 1830s with the passing of the first Vaccination Act,
but the voluntary nature of the Act meant that take-up was poor. A
further Act in 1867 strengthened the legislation. Within seven days
of the birth of a child being registered, the registrar was to
deliver a notice of vaccination; if the child was not presented to
be vaccinated within three months, or brought for inspection
afterwards, the parents or guardians were liable to a summary
conviction and fine of 20 shillings.
Lipscomb’s role in the smallpox vaccination process resulted in the
anti-vaxxers of the day being brought before the magistrates:
James Putnam was next summoned, to show why in several cases he
refused to have his children vaccinated, and said he had a
remarkably fine healthy child vaccinated, and in eleven days she was
a corpse solely in consequence, the doctor certifying that she died
from ‘blood poisoning;’ and when he spoke to Mr. Lipscomb
about the vaccination of the others, he was told by that gentleman
that he would not be answerable that they would not be like the
child which died. He said he could not therefore submit to have his
children vaccinated. He had had twenty summonses in five years, and
had appeared there before them and stated his reasons. He had also
done what he could to get the law altered . . . The Chairman made
the order. Mr. Putnam said ‘it is of no use, I shall not have them
vaccinated.’”
Bucks Herald 20th
June, 1874

The public vaccinator
. . . . and this from the Bucks Herald 18th May, 1878:
“Hannah Baldwin and Elizabeth Norwood, of Tring, were charged by
Mr. Cook, vaccination-officer, at the instance of the Guardians,
with preventing a doctor taking lymph from a child that had been
vaccinated on the 17th ult. Each of them held an infant in her arms,
and were with difficulty made to assent to their having done any
wrong.—Mr. R. N. Lipscomb, surgeon, appeared in support of
the charge, and one of the mothers said he did eight children from
the arm of her infant, and she thought that was enough.—Dr. Lipscomb
said he was the best judge of that.—They were informed that they
were compelled by law to allow of lymph being taken from their
children, and the charge was dismissed.”
After many years of protest compulsory
vaccination was abolished in 1948.
Continuing the theme of smallpox, as part of the fight against this
and other serious infectious disease two hospitals were built near
Tring where patients could be treated in isolation from the rest of
the community, thereby greatly reducing the risk of contagion.
The Aldbury Infectious Diseases Hospital was opened in December
1879. Built by the Berkhamsted Sanitary Authority on an
isolated site in New Ground Road, the hospital was intended for
patients living within the area administered by the Berkhamsted Poor
Law Union, which included Tring. The hospital was managed by
the Sanitary Authority until 1898, when the Aldbury Hospital Joint
Committee ― made up from members of the Berkhamsted and Tring
councils ― took over. However, in 1900 the Tring Urban
District Council decided to build their own isolation hospital.
Lord Rothschild (Lord of the Manor of Tring) offered to donate
a 2½ acre site on Little Tring Road on which to build the hospital, while his wife Emma contributed
towards building and furnishing costs. Designed
by local architect William Huckvale, the Tring Isolation Hospital was opened by Lord Rothschild
on the 19th December 1901. Following the opening the management committees agreed in
principle that scarlet fever and diphtheria patients would be
treated at Tring, and small-pox patients at Aldbury.
――――♦――――
EDWIN JOSEPH LE QUESNE L.R.C.P.L., M.R.C.S.E.
Information on Edwin Le Quesne is sparse. He appears to have
been born at Jersey, Channel Islands,
on the 15th
November, 1851. On the 16th April, 1877, he was admitted
Licentiate of the Royal College of Physicians of London – it appears
that he was residing at the Metropolitan Free Hospital at the time.
On the 13th June, 1881, Le Quesne married Mary Ann Alice. A
notice appears in the Lancet, 9th December 1881, to the effect that
Le Quesne, “Edwin Joseph, L.R.C.P.Lond., M.R.C.S., L.S.A.Lond.,
has been appointed Medical Officer and Public Vaccinator for the
Tring District of the Great Berkhampstead Union, vice Lipscombe,
resigned.”
The Rothschild family acquired Tring Park in 1872, and from then
until his death in 1915, Nathaniel Rothschild, Lord of the Manor of
Tring, was a considerable benefactor to the town. Among other
municipal projects to which he contributed generously were the
construction of the Tring Isolation Hospital and the Tring municipal
cemetery. Lord Rothschild’s wife, Emma, was also a benefactor,
in particular financing the construction of
“Nightingale
House”, the
nursing home that once stood near the end of Station Road on a site
since sold by the N.H.S. for private development. Lady Emma
also contributed generously towards the nursing home’s running costs.
What facilities and services the Nursing Home provided are unclear.
In addition to a district nurse, there are odd clues in press
reports that it also provided services approaching those of a
cottage hospital. Writing in 1940, local historian Arthur
Macdonald Brown states in his book Some
Tring Air
that the nursing home was equipped “with a ward for accidents and
operations”.
Today road traffic accidents are not that uncommon, but even before the age of the motor vehicle
reports of accidents involving ridden horses and horse-drawn
vehicles appear in the press from time-to-time. Usually they
stemmed from panic-prone horses being startled and then bolting out of
control, such as in the following report.
Joseph
Hannell, a tailor from Hemel Hempstead, was one of a party that set
out to visit the Tring Museum riding in
a horse-drawn wagonette. On arrival the horse, a mare, was
stabled at the Castle in Park Road and her headgear taken off.
When the party left for home at 6-30, it appears the mare’s headgear
was not correctly fitted . . . .
“. . . .
They had only proceeded a few yards when a man in the road shouted
that the bit was out of the horse’s mouth. The man approached
the horse, and placing his hand on the straps running over the head,
behind the ears, pulled the bridle over the horse’s head . . . When
the bridle was off the mare started off at once, galloping.
Witness was powerless to stop her, and at the top of the street she
rushed up against the kerb, which caused the wagonette to be
overturned. He recollected nothing further until he found
himself in the Castle, where they were bathing his face. All
the party except Mr. Hannell sen. returned to Hemel Hempstead the
same night. . . . It was not more than twenty yards that the horse
galloped from the gates to the corner where the wagonette overturned
. . . .
. . . .
Mr. Joseph Hannell succumbed on Saturday morning to the injuries he
received in the accident in Park-road the previous Wednesday
evening. By Dr. Le Quesne’s advice he was removed to
the accident ward of the Tring Nursing Home, which, thanks in
a great measure to Lady Rothschild’s wise generosity, is held in
readiness for the reception of such cases. Upon examination it
was found that Mr. Hannell’s spine was broken, with the result that
he was paralysed from the waist downwards. All that medical
science and skilful nursing could accomplish was done to alleviate
the unfortunate man’s sufferings, but from the first it was known
that it was impossible to avert or even delay his death. The
doctor’s efforts were loyally supplemented by
Miss Girardet, the
indefatigable district nurse.”
Bucks Herald 29th September, 1900
An emergency ambulance service, skilled paramedics, accident &
emergency units staffed by specialist in that field, and
ultrasound/X-ray equipment for detecting and examining internal
injuries can now be brought to bear on serious accidents, but none of these facilities were available to Dr. Le Quesne.
The next fatality, which occurred in April 1900, was again caused by
a horse bolting. It happened while a field was being harrowed,
the harrow being drawn by a team of three horses that were being
led by a farm labourer, Shadrach Charles Payne aged 14. At the
inquest into his death it was established that:
“The leader was a young horse. The harrow was attached to the
two hind horses by a chain, which went between them, and the leader
was attached to that chain by two chains and hooks. They had
been at work about an hour and were turning at the end of the field
when one of the rear horses stepped on the leader’s chain.
This horse jumped forward, broke the middle chain, and ran away.
The deceased had hold of a chafe rein and held onto it with his
hand, being dragged ten yards and then falling to the ground.
The chafe rein is a short one, and the deceased was close to the
horse’s head. Deceased fell in front of the horse, which went
right over him.”
The lad being badly hurt was sent home and Dr. Le Quesne was called:
“Mr. Edwin Joseph Le Quesne said he was
a registered medical practitioner, of Tring. On April 12,
about 11a.m., witness visited the deceased, who was up.
Witness assisted to undress him and put him to bed. He
examined him, and found that he was recovering from a state of
collapse. His breathing was laboured and he complained of pain
on the right side. Witness examined his side, but could not
find any mark or bruise, or see that a rib was broken.
Deceased commenced coughing up blood, which suggested injury to the
lung. For a day or two deceased improved, but then he became
worse and his temperature increased. In witness’s opinion he
was suffering from a ruptured lung. Witness last saw him alive
on Thursday evening, but death took place on the following day.
Deceased told him that the horse kicked him, and he considered that
a kick from a horse would produce a rupture of the lung.—The jury
returned a verdict of ‘Accidental death’.”
Bucks Herald 28th April, 1900
Despite the apparent seriousness of the injury there appears to
have been no medical intervention other than observation. The
same applies to the next accident that also involved a bolting horse,
again with fatal consequences. The deceased was a man aged twenty-three.
At the hearing before the coroner the first witness stated that . . .
.
“. . . . on Thursday evening, about 7.15, I
was in the Western-road. I saw the deceased riding a mare in
the direction of Aylesbury. There was a trap coming from the
same direction. I could see that the mare was running away,
and the rider seemed to have lost all control over her. At the
time I saw the deceased he was falling from the mare, and was within
a few yards of me. He fell, his side coming in contact with a
lamp post, and his head striking the ground with great force.
His nose was badly cut by the fall. I went and picked him up,
but he was unable to stand. With assistance I took him to Dr.
Le Quesne‘s surgery. He was conscious, but did not say
anything as to why the mare bolted . . . .
“. . . . Dr. Le Quesne stated — On Thursday evening the
deceased was brought to my surgery, and I saw him on my return about
7.30. I examined him and found his nose broken, and there was
evidence of his having a tremendous blow on the right side, his ribs
being smashed, and there was a fearful contused wound on the right
hip, also internal haemorrhage. He brought up the contents of
his stomach, and from this it was evident that he had not been
drinking. I helped remove him and attended him until his death
at three o’clock on Friday. The cause of death was internal
haemorrhage, the result of injuries occasioned by the fall from the
horse. A verdict was returned accordingly.”
Bucks Herald
15th August, 1891
One forms the impression from this report that an internal
haemorrhage, while evident from the patient’s symptoms, was at the
time untreatable.
Not all Dr. Le Quesne’s appearances in the press involved fatalities.
This report is from the Bucks Herald, 26th November 1895.
“Dr. E. J. Le Quesne, of Tring, is delivering a course of ambulance
lessons to males in the Cheddington School-room on Thursday
evenings. Judging by the number of workmen who attend, at
least this form of technical instruction, promoted by Bucks. County
Council, is appreciated.”
Dr. Le Quesne lived
for at least part of his time in Tring at Elm House, the large property that stands in its own grounds at
the junction of Tring High Street and Langdon Street.
An auction advertisement for the sale of his furniture suggests that
Dr. Le Quesne left the town around 1910 and retired to Jersey. He died at “Melbury,” Havre des Pas, Jersey in his 68th year
on the 24th January 1919.
――――♦――――
JAMES BROWN M.B., C.M.Edin.
Judging by his qualifications – Bachelor of Medicine, Master of
Surgery (Chirurgiae Magistrum)
– James Brown was the first university educated medical
practitioner in Tring, his predecessors having progressed through
the earlier apprenticeship route. Brown came to Tring c.1884, first
as assistant to Mr. Pope, then as his partner. On Pope’s
retirement, Brown took over the practice. In addition to his
medical duties he was also a long-serving member of the Urban
District Council where his opinions and advice, especially upon
questions affecting the health and sanitation in the district, were
highly valued. Dr. Brown married Miss Fulton, a sister of the wife
of Richardson Carr, agent to Lord Rothschild, and they lived at the
large house called
“Harvieston” on Aylesbury Road.

Harvieston,
Dr. Brown’s residence.
In the age proceeding the motor car, local G.P.s travelled among
their rural patients on horseback or in a horse-drawn vehicle.
This meant that besides having to maintain a horse, a
groom-cum-coachman was also needed to ensure that the doctor’s
transport was available when he required it. In his memoir
Medicine in Tring, Dr. Thalon recalled that for many years a speaking tube ran from the
doctor’s house at No. 23 High Street to the groom’s room on the
other side of the road. This was used when the doctor was
called out at night and the groom had to get the horse and carriage
ready; and horses, being creatures prone to panic, sometimes bolted
causing a spill:
“ACCIDENT TO DR. BROWN.―We are sorry to record that Dr. Brown had an unfortunate spill
near Aldbury on Sunday morning when out on professional business.
The horse, frightened, it is thought, by some sheep, reared and
threw both Dr. Brown and his coachman out. The doctor was
severely shaken and bruised, but Bruce
[his coachman] unfortunately dislocated his collar-bone. We are pleased
to say the doctor is about again and Bruce is making satisfactory
progress.”
Bucks Herald 6th October, 1900
Returning to serious infectious disease, following an outbreak of
smallpox in 1902, accommodation at the Aldbury Isolation Hospital
came under pressure:
“HOSPITAL
ACCOMMODATION.―
In view of the fact that five smallpox patients were already in
Aldbury Hospital, which only contained eight beds, the Council
considered the question of providing additional accommodation if
necessary. A representative from Messrs. Humphries, Knightsbridge,
attended the meeting, and gave particulars as to the cost etc., of
erecting temporary iron buildings on the grounds of the Aldbury
Hospital, permission for which had been given by the Aldbury Joint
Committee. Two perfectly plain blocks, 40 feet by 20 feet,
would cost about £170, and a wood foundation would be about £10 extra.
These in the opinion of Dr. Brown would be quite suitable.
It was resolved ‘That the Hospital Committee be empowered to act in
dealing with the erection of temporary buildings and in other ways
with the smallpox outbreak.’”
Bucks Herald 29th March, 1902
Following the opening of the Tring Isolation Hospital in 1901,
permission for friends/families to visit patients
in isolation, especially children, became a bone of contention
with those administering the hospital – visiting
appears to have been an existing problem at the older Aldbury
hospital:
“THE
ISOLATION
HOSPITAL.–
On Saturday the scarlet fever patients in the Aldbury Hospital were
removed to the new isolation hospital belonging to the Tring Urban
District Council, and the Aldbury building was prepared for the
reception of some cases which were suspected to be smallpox.
On Sunday afternoon several persons who had been accustomed to go to
the Aldbury Hospital to see their children or friends through the
window presented themselves at the new hospital gate, but were
informed by the porter that the doctor had given orders that no one
was to be admitted without an order from him. Two or three of
the men started for Tring to get the necessary permit, but were told
by Dr. Brown that the Hospital Committee had decided that no
visitors were to be permitted within the hospital grounds.
Great dissatisfaction was expressed at this departure from the rule
which had so long obtained at Aldbury.”
Bucks Herald 18th January, 1902
“Dr.
Brown: To allow visiting does away with the whole idea of an
isolation hospital. At Aldbury we have a lot of trouble with
visitors, for if we do not watch the whole of the time they had the
windows open or were popping through the doors . . . . It was
eventually decided that words to the effect that parents would be
allowed to visit their children who were seriously ill should be
added to the rules.”
Bucks Herald 15th February, 1902
Besides his administrative work on hospital committees, Dr. Brown also
encountered serious disease in his everyday role as a medical
practitioner:
“A CASE
OF
SMALLPOX.–
On Tuesday a case of smallpox was notified in Tring. A young
man named George Norwood, living at 26, Albert Street, but working
with a gang on the railway cutting near Haddenham in the adjoining
county of Bucks, returned to his home on Monday ill. On
Tuesday morning he was seen by Dr. Brown, who thought his
symptoms pointed to smallpox. The doctor at once communicated
with the Medical Officer for the district, Dr. W. Gruggen
[of
whom more later], by whose
direction Norwood was the same evening conveyed to the Isolation
Hospital at Aldbury. The two other occupants of the house in
Albert Street were put in quarantine, and everything was done to
prevent the spread of the disease. As the patient had not been
in contact with anyone outside his home, there was every reason to
hope that, thanks to the prompt action of Dr. Brown and the
Medical Officer, the infection will not spread.”
Bucks Herald 21st March,
1903
In the
next case the coroner for the district held an inquiry into the
death of Tom Briant, a Tring postman aged 56 who was hard of
hearing. This is an early road traffic accident in the town involving a
motor vehicle, and one that would probably be viewed more critically
by today’s traffic police than by the town’s police force of 1912.
When interviewed by the police the car’s driver, an Aylesbury
dentist, said he saw Briant in the road gathering manure into a
bucket. When asked why he did not stop the driver replied that
having sounded his horn he thought the man was going to move out of
the way, but not having heard the horn Briant stepped into the path
of the car. He was then struck by the car’s nearside wing and,
despite one witness claiming the car was travelling at no more than
10 m.p.h., the vehicle pushed Briant along the road for 12 yards
before stopping:
“. . . . P.C.
Endersby, stationed at Tring said he received information of the
accident about 11.40 on the morning of March 7th. He went at
once, and found deceased lying in the road, and the car on the
right-hand side of the road about 8 inches from the path. The
road was about 16 feet wide at this point. Witness assisted
the doctor to move deceased, who seemed dazed. He said he
never saw or heard the car till he was knocked down, when he
clutched the front of the car. Deceased was apparently pushed
along about 12 yards by the car.
By Mr.
Wilkins
[witness]
― He could see where the dust had been pushed up by the deceased
being shoved along . . . .
. . . . Dr. Brown said he received a telegram about 12.25 at
Aldbury, and got to Mr. Briant’s house about one o’clock. He
found deceased had a fracture of the left thigh, about the middle of
the lower third; and also slight bruises on the right hip and
thigh. It was rather a troublesome fracture to set, and
chloroform had to be administered. Dr. O’Keeffe
assisted to set the leg. There was very little trouble with
the leg after it was set. Witness had attended deceased for 27
years. He had weak heart muscles. Between the 7th and
the 20th there were no drawbacks, except the discomfort of changing
the splints. On the morning of the 20th deceased was very
well. He said he had not been better for years. About 10
the some night witness was fetched, but found deceased dead when he
got there. From the description of the symptoms he got from
the daughter, he should say death was caused by a clot of blood in
the pulmonary artery. This was not an uncommon thing to happen
after an injury or an accident.”
Bucks Herald 30th March, 1912
The jury
returned a verdict that death was due to a blood clot in the
pulmonary artery, the result of being laid up with injuries
sustained in the occurrence which was purely accidental.
James Brown died on the 15th December 1914 at his home “Harvieston”
on the Aylesbury Road.
He had lived Tring
for some twenty-five years, during which time “his assiduous attention to his
professional duties, and his courteous bearing to all, made him
popular with all classes. His work as a doctor naturally
brought him much into contact with his poorer neighbours, and his
kindness and sympathetic consideration for the humblest of them won
for him their lasting esteem.” He left a widow and three
children, two daughters and a son,
Andrew,
who
was killed in action on the 2nd July 1916 while serving as a second
lieutenant in the South Staffordshire Regiment.
――――♦――――
WILLIAM WARD ANDERSON M.B., B.Ch. Edin.
Dr. Anderson qualified at Edinburgh University
in July 1904
with the degrees of Batchelor of Medicine and Bachelor of Surgery
(Ch = Chirurgie, Latin for surgery). The 1908 edition of
Kelly’s Directory for Tring lists him in partnership with Dr. Le
Quesne, their practice being in Western Road (possibly Le Quesne’s
residence at Elm House).
A local doctor being called
out in connection with a murder is unusual, particularly so when the
victim is an infant. This case involved a boy aged about 14 months
whose body was discovered weighed down with a brick in a
well at Buckland. Dr. Anderson was called upon to establish
the cause of death:
“Dr. W. Ward Anderson, practising at Tring, deposed that in response to
a message from P.C. Wicks he went to Drayton Mead Farm on November
27 and saw the body of an infant child lying in an outhouse.
On his instructions P.C. Wicks undressed it. It was a male
child, quite dead; rigor mortis had passed off, and the body was
very much swollen. The child had been vaccinated. On
Wednesday he made a post-mortem examination and found that there
were ten teeth, indicating an age of a year to 14 months. The
heart chambers were empty, and the muscles of the heart pale in
colour. There was no disease. The lungs were swollen and
contained a mixture of air and water on the surface, and were
spongy. The other organs were healthy and the body had been
well nourished and cared for. All the limbs were normal, and
there was no sign of any poison. From the condition of the
lungs he formed the opinion that the child died from suffocation as
the result of immersion in water. He thought it had been in
the water about seven or eight weeks. He was quite satisfied
that it was alive when it entered the water. After the body
had been in the water a considerable time it would become swollen
with decomposing gases, and then become buoyant and able to lift a
weight in the water. He thought the body would probably rise
to the top of the water, if it had the brick produced attached to
it, in about a month. The stains on the clothing probably
arose from some iron in the water.”
Bucks Herald 1st December, 1917
The child’s mother was eventually traced. Her name was
Dora Edith Scott, she was twenty-six years of age, homeless, and
working in a munitions factory at Watford. Having been taken
into custody she made the following statement to the arresting
police officer:
“I couldn’t get anyone to look after it
[her infant].
I tried at ever so many places. I tried the day nursery, but
they were full up, and Mrs. Went, who I was living with, said she
couldn’t look after it any longer, as she was not well herself and
had one baby of her own. So I told Mrs. Went that I would try
and get it somewhere else. And I went, and I am sorry to say
that I had a little drop of drink that afternoon, as it drove me to
drink. I got down-hearted, and I did away with him. I
did not know what I was doing, or I should not have done it. I
have no husband. He died before the war, and this child
belongs to a soldier. The soldier took advantage of me, and I
had the child. I saw no more of him, and have not heard of him
since before the child was born. I have one child by my own
husband, which my mother has got. My mother lives at Whelpley
Hill, but she would not have this one, as the other is too much for
her. My husband has been dead six years. He was a native
of Chorlywood, and we lived there. The child’s name was
Cyril.”
Bucks Herald, 19th January, 1918
Dora Edith Scott
Following her statement,
Edith was charged with murder and taken into custody. She was later tried for murder at the Bucks Assizes, found guilty, and
sentenced to death. However, thanks to her solicitor (Mr. R.
S. Wood of High Wycombe) who presented a petition to the Home
Secretary, her sentence was commuted to “penal servitude for life.”
What became of Dr. Anderson is something of a mystery. In September 1918 a
notice appeared in the Bucks Herald informing patients that
he had moved his consulting room from Western Road to Clifton House,
Frogmore Street. After that – to the extent that he can be
clearly identified –
his last entry in the local press is in September 1920 when a
notice was published informing readers that Dr. Anderson’s seat on
Tring Town Council had been declared vacant due to his unexplained
absence at meetings during the preceding six months. The
British Medical Journal lists a William Ward Anderson as having died
on the 10th November, 1955.
――――♦――――
CHARLES EDWARD O’KEEFFE L.R.C.P. & S.I.
There’s a dearth of biographical information on Dr. O'Keeffe.
What there is comes from the pen of his former colleague, David Thallon:
“He
(Dr. O’Keeffe) and Dr Norman Knox, together with Dr
Christopher Cole, whose family lived in Tring for several
generations, were in partnership until the beginning of the NHS in
1948. Dr O’Keeffe was, I understand, someone who inspired
great confidence and had a wonderful bedside manner. He
treated the more well-off section of the community, while his
partner, Dr Carpenter, dealt with the rest. Lord Rothschild
[Walter Rothschild], who was one of Dr O’Keefe’s patients, required him to visit
every day. He was one of the first people in Tring to own a
motor car, having previously used a motorbike to do his visits.”
The cases involving physical violence so far referred
to have been pugilistic contests where it is reasonable to assume
that the participants were willing. The next case is very
different, and although the assailant –
Percy John Eggleton of Miswell Farm
–
was eventually convicted of malicious wounding, the Bucks Herald
report suggests that he nearly faced a charge of wilful murder:
“Dr. C. E. O’Keeffe, Tring, said he was called to the
Icknield Way about 4.30 p.m. on Sept. 11, and found a woman lying by
the side of the road on her back and unconscious. Both eyes
were closed, and she was bleeding from the head. On his
instructions she was removed to the Tring Nursing Home, where he
examined her, and found extensive bruises and cuts about the head,
such as might have have been caused by the stone produced. In
consequence of her serious condition he thought it advisable to have
her removed to the Royal Bucks Hospital at Aylesbury, and she was
conveyed thither on the following day. She then developed
the rigidity of paralysis on the right side, and was still unconscious.
When he examined her on the Icknield Way he noticed blood stains on
her underclothing. At the time he sent her to Aylesbury her
injuries were of such a nature that he was doubtful if she would
recover.”
Bucks Herald 8th November, 1918
Having been identified,
Eggleton was brought to trial at the Herts. Assizes charged with maliciously
wounding Susan Carter. During the trial prosecuting counsel
had this to say . . . .
“. . .
. it was as bad and brutal an assault as his Lordship had ever had
to try. Prisoner dashed out on the high road where this poor
old woman of sixty years was walking, set upon her, and inflicted
such terrible injuries that for a time her life was despaired of.
The best opinion the doctors could give was that she would never
recover from the blows she received. There was no evidence to
show what weapon was used.”
Bucks Herald 21st November, 1919
Eggleton was sentenced to 18 months imprisonment with hard labour.
In December, 1940,
Home Farm was taken over for maternity care after the Lambeth
Municipal Maternity Home had been destroyed by bombing. On the 1st June, 1945, the Tring facility announced that the
1,000th baby had been born there.
Located in Park Road,
Home Farm Emergency Maternity Home was run by the staff from the Lambeth Municipal Maternity Home.
Its clientele were mainly cases sent to Tring by the London
County Council, but it also received evacuated mothers-to-be who
were billeted in the neighbourhood and it appears to have catered for
some at least of the town’s residents.
During the coroner’s hearings referred to in previous cases, medical evidence
concerning cause of death had been accepted without question. However,
in the following case – which involved death in childbirth
–
Dr. O’Keeffe
was questioned by a barrister representing the
husband and mother of the deceased woman, Vera Mary Catherine Rees
(aged 25), who appear to have suspected that Vera’s death may have
resulted from negligence:
“Dr. C. E. O’Keeffe, of Tring, gave evidence that it was a
very difficult labour; the child, which was born dead, weighing over
10lbs., which was very large, especially for a firstborn.
The mother was given a safe dose of chloroform. After the
child was born Mrs. Rees ceased to breathe. He applied
artificial respiration and she started to breathe again, but she
again relapsed. He continued artificial respiration and gave
some injections into her heart, to try and stimulate the heart, but
these had no effect . . . . He had no doubt that her kidneys,
although they showed no evidence of disorder previous to her labour,
were not doing their work properly during the last hours of her
life. She was suffering from a poisoning condition from her
kidneys, although there was a satisfactory test before her
confinement . . . . In reply to lengthy and detailed questioning by
Mr. Figg, Dr. O’Keeffe stated that although Mrs. Rees entered
the home on May 10th and the birth did not take place till the 16th,
it was a perfectly straightforward case. He had known plenty
of women in labour for a week without any complications.”
Bucks Herald 26th May, 1944
The coroner concluded that death was due to heart failure from
the causes outlined in the medical evidence, and he could not see
that there was any negligence on anybody’s part. It is
interesting to note in passing that chloroform, which was given to
Vera, is no longer used as an anaesthetic due to
the relatively high risk of complications, including possible heart
failure.
Bucks Herald 8th
March 1963. Dr. O’Keeffe obituary.
“Dr Charles Edward O’Keefe who
practised in Tring for many years died on Friday aged 83. His
home was Stud Farm, West Leith, Tring. Born in County Cork,
Ireland, he trained in Dublin, qualified in 1902, came to Tring on
January 1st 1905 and joined practice with the late Dr Brown.
When Dr Brown died, he took over the practice and was later joined
by Dr. H. N. Knox. Dr O’Keefe served as captain in the RAMC in
WWI. He is survived by his wife who is a former Tring
Councillor and two daughters, Mrs Helen Walford and Miss Bridget
O’Keefe who is in practice near Norwich. Funeral was at Tring
Church on Wednesday.”
――――♦――――
HENRY NORMAN KNOX M.R.C.S.Eng., L.R.C.P.Lond.
Henry Norman Knox was born at Dunedin, New Zealand, in 1898.
During the First World War he served with the Durban Light Infantry
in German West Africa. In 1922 he commenced his medical
studies at King’s College Hospital, London, graduating in 1928.
He later served at King’s as House Physician and Senior Resident
Accoucheur. In 1930, he joined an old-established practice at
Tring, later becoming Senior Partner until his retirement in 1962.
The founding principles of the National Health Service (NHS) were
that health services should be comprehensive, universal and free at
the point of delivery — a health service based on clinical need, not
ability to pay. The first case involving Dr. Knox, illustrates how
ability to pay was a serious concern at local level before the NHS
was established in 1948. It concerns a patient at the Tring
Isolation Hospital who contracted double acute mastoiditis [10], a
serious condition that required expensive surgery. The Chairman
of the Tring Council felt obliged to accept the charge for the
procedures without
the formal authority to do so:
“The Clerk [of
the Council] had received a letter from
from Dr. H. N. Knox, of Tring, regarding the case of Patricia
Ward, now discharged from the Isolation Hospital at Tring. He
wrote ‘Her complications, double acute mastoiditis, are liable to
occur in any infectious case, and necessitate an immediate
operation. In her case Dr. Steele was called in and operated
in the emergency. His charges are not small, if reasonable.
I feel that if in future cases of this description should arise the
doctor in charge should be able to call in a London specialist,
whose charges would be the same.’
Dr. Knox referred to the necessity of immediate action in
such cases, and suggested that the Council should appoint some
person who could be consulted first as to action on such an
occasion. He said ‘I went to great trouble in this recent
case, giving my time and help in making all arrangements. My
remuneration was nil, except the usual fee. . . No Tring patient has
required such an operation before, and it is hoped the occasion will
not arise again.’
The Clerk stated some arrangement was required in case of sudden
emergency such as the one referred to. In this case they were
fortunately able to get to the child at once, and the Chairman was
faced with the difficulty of making up his mind in authorising the
operation to be done. He could not say what the fee would be.
The Chairman had to shoulder the whole responsibility, not knowing
what the charge would be to the Council. It did cause even
some delay, which was very dangerous in these cases.”
Bucks Herald on the 6th October 1933
At the meeting the Council voted to authorise the Chairman, or
Vice-Chairman, or Clerk to act in future on such occasions.
A coroner’s inquest held at Aylesbury in 1941 referred to Ernest Foulton of Buckland Common who, suffering from prolonged intractable pain, took his own life:
“Mrs. Nellie Ada Fulton, wife of the deceased man, said that her
husband, who was 47 years of age, was by occupation a labourer.
He had been ill for some time and had undergone three operations,
the last one was four years ago. He had been attended by Dr.
Knox, of Tring. Lately he had been in bed and complained of
terrible pain in his side and he told her that the pain was getting
worse . . . . Her husband possessed a double-barrelled gun which was
kept in the front room together with cartridges.
Mrs. Elizabeth Victor Penn . . . . said that at about 9 o’clock she
heard a gun shot . . . . She opened her door and saw Mr. Fulton
lying on the garden path, with a gun, outside his house . . . .
Witness could see that he was wounded in the side.
Dr. Henry Norman Knox, of Tring, stated that Mr. Fulton had
been a patient of his for 11 years. In 1925 he was operated on
for internal ulcer. The operation was not a success and he had
been operated on twice afterwards. He was able to get up
again, but suffered from arthritis and had serious abdominal pain
and pain in the legs. The deceased man had asked if he could
be operated upon again, but X-ray examination revealed that any
further operation could do no good in his case. Recently he
complained of the pain getting worse and witness had administered
small doses of morphia when the pain had grown worse. Foulton
had expressed the wish that he could be out of it all, but he never
threatened to do anything to himself . . . .
Rose Coles, district nurse, Buckland Common, said that she
accompanied Foulton to the Royal Bucks Hospital in the ambulance and
administered oxygen on the journey. But the man died on the
way. She knew Foulton, who had complained to her greatly of
his pain . . . .”
Bucks Herald 10th January, 1941
The Coroner recorded a verdict that death was due to an injury,
self-inflicted whilst the balance of the deceased’s mind was
disturbed.
Tetanus, often referred to as “lockjaw” after its most recognisable
early symptom, is a bacterial disease that affects the brain and the nervous system.
The bacteria, which
usually enters the body through cuts or grazes, is
commonly found in soil and the manure of animals such as
horses and cows. Although there is no cure for the disease,
treatments are available for managing its symptoms and complications
until they disappear. However, the best way to protect against
tetanus is to take the vaccine. Immunisation was introduced in
some localities as part of the primary immunisation of infants
from the mid-1950s, then nationally in 1961. Occurrences of the disease in the
U.K. are now rare.
In this
coroner’s hearing
it was concluded that
tetanus infection probably entered the victim through an abrasion on
his thumb. The victim, George Puddefoot, a 25-year-old farm
labourer, returned home from work on Thursday the 10th April
at 5.30 p.m
. . . .
“. . . . and then said that his back was
bad, that he ached from the bottom of his back up to his shoulder.
He did not suggest the cause of it. After she
[his mother] had
examined and well rubbed his back with liniment she advised him to
go to bed.
She visited him during the night. He had a very restless
night. During the following day she rubbed his back, but it
did not improve, and he was restless the following night. On
Saturday morning she called in Dr. Knox, of Tring, who
advised his removal to the Grove
[Isolation] Hospital, and this was done. Her son was removed from
Grove Hospital to the Royal Bucks Hospital on Tuesday, April 15th.
Dr. M. C. Rothcope, Bridge House, Leighton Road, Linslade, medical
officer of Grove Isolation Hospital, stated that on Saturday, April
12th, Puddefoot was admitted at the hospital, with a medical report
of suspected cerebro-spinal meningitis . . . . Witness drew off some
spinal fluid for laboratory examination and gave him an injection of
anti-tetanus serum. Puddefoot was also given other treatment, in
case there was any cerebro-spinal infection. On the following
Monday there was some evidence of stiffness of the jaw and muscles.
The report received on the morning of April 15th showed that there
were no germs of cerebro-spinal meningitis. Puddefoot was given a
further injection of anti-tetanus serum and arrangements were made
for his removal to the Royal Bucks Hospital, in case further
investigations were required. He was removed the same day.
Dr. R. K. I. Kennedy, resident medical officer at the Royal Bucks
Hospital, stated that on April 16th Puddefoot was in a state of
tetanic spasm
[11] and could not open his jaw at all. He was given the appropriate
treatment, but became worse and died on Wednesday, April 16th. There
was a small abrasion at the base of the left thumb-nail and a small
superficial scratch on the left wrist . . . . Death was due to the
tetanus, the most probable point of entry of the bacilli might have
been the abrasion at the base of the left thumb-nail.”
Bucks Herald 25th April, 1941
Dr. Knox retired after 32 years and was able to enjoy his family,
his golf, and his garden for a further 23 years. His kitchen
garden was perfection and a source of much pride to him.
He lived at Bell View in Park Road and died there on the 6th March, 1985, aged 87 years.
――――♦――――
EDWARD MIDDLETON-BROWN B.A., M.D., L.R.C.P., M.R.C.S.
In his
memoir of
Tring’s doctors, Dr. Thallon says that:
“There were, of course, other medical practices in the town during
this time, notably Dr Middleton-Brown. He practiced from a
surgery close to the United Reform church in the High Street.
He was considered very high class and had a French wife as well as
three daughters, who were heavily chaperoned.”
Edward Middleton-Brown was born on the 1st May 1879 at Barnstable,
Devon. At an early age he appears to have changed career direction, for having
taken a B.A. degree in 1900, he then went on to acquire the medical
qualifications of B.C. (Batchelor of Surgery, C = Chirurgie, Latin for surgery) in 1904,
M.B. (Batchelor of Medicine) in 1905 and M.D. (Doctor of Medicine) in 1921. During the First World War he
served as a Captain in the Royal Army Medical Corps. The earliest
reference to Middleton-Brown in the press suggests that he came to
Tring c.1920, a notice in the Bucks Herald dated 24th
April, 1920 reading . . . .
“Dr. E. Middleton-Brown has been appointed vaccination officer for
the district of Tring.”
In the next case the deceased, John Cutler, was a builder’s labourer aged
44. On March 10th he was working at a building site in Grove
Road, Tring, when a slab he was helping to move broke, injuring his
thumb. Dr. Knox stitched the wound, and Cutler returned to
work. Towards the end of the month he complained of a pain in
his back that had become progressively worse.
On Sunday the 2nd April
Dr. Middleton-Brown was
sent for, and on the following day he removed Cutler to the Royal Bucks Hospital. By Saturday Cutler
was complaining of increased pain and he died that evening, his wife
being with him:
“Dr. E. Middleton Brown, Tring, said that he had known Cutler for
some years, and his general state of health was quite good. On
March 10th deceased called at his surgery and told and told him he
had crushed his thumb whilst he was handling a slab. Witness
redressed the wound, which was a lacerated wound round the inner
margin of the thumb, and bruising of the base of the thumbnail. He
told him to continue to dress it with boracic lint. It did not show
any signs of being septic. Witness advised him not to continue work,
but Cutler replied that it was his left thumb, and he was unwilling
to give up his work. On subsequent occasions Cutler visited the
surgery and the thumb appeared to be healing very satisfactorily. On
Sunday, April 2nd, witness was called to Cutler’s home. Deceased
complained of stiffness and pain in the lower region of his back. He
thought that at the time Cutler had got lumbago, and certain
treatment was prescribed and he was advised to stay in bed. On April
3rd he saw him again, and he complained of his back and neck being
stiff and contracted. The rigidity was very much more marked and
became general, and he suspected tetanus. He got his partner to
confirm his diagnosis and sent him to the Royal Bucks Hospital.
Witness suspected the tetanus was derived from the wound on the
thumb, as tetanus usually entered through an open wound . . . .
. . . . Dr. A. A. Miller,
house surgeon, Royal Bucks Hospital, Aylesbury, stated that he saw
deceased on admission. The top of the wound appeared to be in a
gangrenous condition. Dealing with his general condition, he said
that deceased was unable to open his mouth. His neck muscles
were in a similar state, whilst the back and lower limbs were very
rigid. Under the anaesthetic the wound was thoroughly cleaned
and tetanus anti-toxin was injected. On April 6th his general
condition became much worse and his spasms of tetanus were more
frequent. On the next day he was in a very critical condition,
and on Saturday he was visibly down, and he died at 11.55 p.m.
In witness’s opinion death was due to acute tetanus, which arose
from the injury to his thumb. The tetanus, germ had got into
the blood through the wound in the thumb.”
Bucks Herald
14th April 1933
Having being satisfied that tetanus was its cause, the recorder returned a verdict of
accidental death.
Although his practice was
“considered
very high class,” Dr. Middelton-Brown was also involved in police work,
such as in this case
of death by misadventure.
The deceased was Miss Lydia Mary Wake of Goldfield Mill House,
Tring. Her servant, on returning home from an outing couldn’t
locate her mistress. On searching the
house she discovered that the bathroom door was locked and unable to receive an answer she called
in a neighbour who forced the door. Miss Wake
was found lying face down and partly submerged in the bath, dead. The police and
a doctor were called.
“Dr. Middleton Brown of Tring said he had never attended
the deceased professionally. He was called at 6.5 p.m. on Monday by P.S. Lee to go to Mr. Richard’s house and there he saw deceased
lying in a bath face downwards, covered with a towel, and wearing a
rubber cap, which had slipped down almost on to the bridge of the
nose. The nose was resting against the sloping end of the hath. Both
arms were bent under the body and the legs bent upwards, the bath
being too short for the body to be fully extended. Underneath the
body were a piece of soap and a flannel. There were no marks of
violence on the body. She had been dead from three to four hours. The body was quite well-nourished and there were no signs of
illness, or operation scars. P.S. Lee assisted witness in getting
the body from the bath and artificial respiration was tried without
success. The primary cause of death was syncope followed by
asphyxiation due to drowning. Deceased probably became faint from
trouble with the heart, or anaemia of the brain, the head then
dropped below the level of the water, through collapse, which would
cause drowning. Deceased’s face was blue and there was froth at the
lips, and she had the appearance of having been drowned. The
possible explanation of deceased being face downwards was that she
had struggled to reach a bell in the wall which was quite close to
the sloping end of the bath, and that she fell because of being
faint.”
Bucks Herald 26th April, 1924
While there may have been a suspicion of suicide in this
case, in the next case death was clearly self-inflicted:
“Dearest Marion.—Forgive me. I cannot endure longer. Please thank
ever body.—Your broken-hearted Fred.”
This poignant farewell was found written in a loose-leaf notebook on
the body of Frederick George Evans, a 45-year-old commercial
salesman, which was found lying dead in Stubbings Wood, near Tring:
“Dr. Middleton Brown, the police
surgeon, deposed to seeing the deceased lying on a bank in Stubbings
Wood. The body was fully clothed with the exception of the
hat, which was lying nearby. The legs and arms were extended
and there was a dark stain round the mouth which extended over the
chin down the throat. Inside an attaché case (produced), which
was lying near the body, was a 16oz. bottle of Lysol and a cup.
The stains round the mouth looked as though they had been made by a
corrosive fluid such as Lysol.
The Coroner: If deceased had taken neat Lysol would it have taken
much to kill him? — No, not very much.
Continuing, Dr. Brown said deceased was clutching the grass with one
hand and must have suffered a great deal of pain. Witness was
absolutely satisfied that deceased had taken Lysol, and the cause of
death was shock.”
Bucks Herald 22nd July, 1932
Although Evans was known to be worried about business matters he had
never threatened to take his own life. However, at the inquest
held in the Market House Tring, a verdict of “Suicide during
temporary insanity” was returned.
Dr. Middleton-Brown
left Tring in
1956. He died at the Cottage Hospital, Marlow, in 1960 aged
81, being survived by a widow and three daughters.
――――♦――――
MEDICAL OFFICERS OF HEALTH
The doctors referred to in this paper so far have all been general
practitioners (or their earlier equivalents). Although
Medical Officers of Health
did not treat patients
individually, they were of equal importance to the community, particularly at
a time when the town’s sanitation [12] was of a very poor standard.
Although the cause of cholera was at the time unknown, the epidemics
that attacked Britain during the 1830s and 1840s spawned what became
a public health service. Local Boards of Health were formed to
place water supply; sewerage; drainage; cleansing; paving, and
environmental health regulation under a single local body. An
important role that grew out of these changes was that of Medical
Officer of Health (MOH), a role that was to play an
important part in tackling environmental health issues in the second
half of the nineteenth century. In 1856, the MOH for Bethnal
Green, London, described his role thus:
“The Instructions to Medical Officers of Health direct them to
inquire into, and to report, periodically, upon the physical
conditions of the place and people, their vital statistics and
sanitary state, the ventilation and drainage of houses, the drinking
waters and water supply, the condition of the burial grounds,
slaughtering places, and homes of the industrial classes, and to
state, on referring to existing evils, what sanitary appliances are
best for their mitigation.”
――――♦――――
CHARLES EDWARD SAUNDERS M.D. Aberd., M.R.C.P.Lond., D.P.H.Camb.
Dr. Saunders was Medical Officer of Health for Middlesex and
Hertfordshire, an area that included Tring.
The problems that appear to have been of most concern in Tring
were the faecal pollution of drinking water and lack of an effective
means for disposing of human faecal matter and sewage. On this latter concern, in 1877 Dr. Saunders
published a report on the sanitary ― or rather insanitary ―
conditions prevailing in parts of the town in which he refers to
squalor that now makes disturbing reading. On the need for the
town to acquire an effective means of sewage disposal he had this to
say:
“This necessity can scarcely by better appreciated than by comparing
two streets in the Western Road ― Charles Street and Langdon Street
― the one with pail privies, emptied into an open ashpit and having
slop-water cesspools; the other having a sewer into which many of
its houses can, and do, drain. The filth and squalor of the
one and the decency and order of the other could scarcely fail to
show the necessity for a better system of filth removal.
Another place I would refer to is Church Alley. Here there is
a row of 10 privies within about 8 feet of the back-doors of the
houses; these privies have pails, and these pails when full, as they
usually have been when I have seen them, are emptied into a huge
ashpit, also near the back-doors of the houses.”
Sanitary Conditions of Middlesex and
Hertfordshire for the year 1877.
When in 1867 the Council first attempted to introduce a system of
sewage disposal, not only did it divert water that previously had
been used to maintain the level of the Grand Junction Canal as it
crossed the Chilterns, but the town’s human waste was deposited in the
local canal reservoir. Much angered by this, the Canal Company
applied for an injunction against Tring Council to cease the
nuisance. This, the Council opposed, but the canal company won
their injunction. Dr. Saunders had this to say about the
failed scheme:
“The Board’s
[Town Council’s] first attempt to carry out a scheme of sewage was so singularly
disastrous that their efforts for the last five years have been
confined to devising means to undo the mischief that was done . . .
.
Sanitary Conditions of Middlesex and Hertfordshire for the year
1877.
It’s not clear when exactly Tring acquired an effective sewage
disposal system, but news reports suggest it was early in the 1880s.
Dr. Saunders later became Superintendent of the Sussex County Asylum
at Haywards Heath. He died in 1904 following a period of
failing health.
――――♦――――
WILLIAM GRUGGEN L.K.Q.C.P.Irel. & L.M., L.F.P.S.Glas.,
P.H.Dip.Camb.
William Gruggen was appointed Medical Officer of Health to the Local Board
(i.e. Town Council) in 1890. It was a time in which Tring
was undergoing significant improvements in sanitation, especially to
the provision of clean drinking water and effective sewage disposal.
In line with the
Instructions to Medical Officers of Health
referred to earlier, Dr. Gruggen reported periodically on the
sanitary conditions that he found in the course of his work.
The following extract, taken from the Bucks Herald,
sets out his concerns over poor sanitation
and its causal link to the
1891/92 diphtheria outbreak in Tring:
“The enumerated population of this district is 4,525. During the
past year 78 deaths occurred. Of these, 13 were of children
under one year of age and 30 of persons over 60. Zymotic disease
[13] caused 12 deaths — 11 from diphtheria and one from diarrhoea.
The death rate (after adding the deaths in the Workhouse at
Berkhamsted, belonging to the district) is 17.9 per thousand living.
There were 127 births registered during the year, giving a
birth-rate of 25.8 per thousand living. The deaths of children
under one year of age were in the proportion of 102.3 to a thousand
births. This is a considerable improvement upon last year,
which itself was better than any year since 1886.
The zymotic death-rate is 2.6 per thousand living. This high
rate was caused by a serious epidemic of diphtheria which occurred
in the town during the latter part of the year. Referring to the
diphtheria outbreak, Dr. Gruggen states that he had called
attention to ‘The unsatisfactory state of the water-closets, from
being without a proper water supply. In hardly any of the
closets is water laid on for flushing, hand flushing being relied
on, with the result that in most cases they were abominably filthy,
and I would in all seriousness and with all respect again call the
attention of the Authority to this matter, which in one worthy of
their earnest attention.
Another point which I wish to mention is the badly paved end filthy
condition of many of the yards attached to the houses in the town.
Puddles of filthy water are to be seen in all directions in these
ill-paved surroundings, and it is utterly impossible, were the
people ever so willing, to keep these yards decently clean.
There being reason to believe that the germs of diphtheria may find
a habitation in a filth-laden soil, and being forced out with the
ground air by a rise in the ground water, the necessity for the
proper paving, and rendering impervious to air and moisture of the
grounds in connection with the dwellings, at once becomes apparent.
Under section 23 of the Public Health Acts Amendment Act, 1890,
section 157 of the Public Health Act, 1878, has been extended so as
to empower every Urban Sanitary Authority to make bye-laws with
respect to the paving of yards and open spaces in connection with
dwelling houses: and I would submit that this matter also merits the
serious attention of the Authority. Eight samples of water
were sent to me for analysis, of which two were good, one bad, and
five doubtful.’”
Bucks Herald 28th May
1892
Serious epidemics remained relatively common in an age before
vaccination against such diseases as diphtheria were available and
freely given, the diphtheria epidemic that Dr. Gruggen refers to his
report being an example (a serious
typhoid epidemic followed in 1899).
Diphtheria is a potentially fatal contagious bacterial infection.
It is dangerous because the bacteria that cause it produce a
powerful toxin (poison) that kills cells in the mouth, nose and
throat. These dead cells accumulate to form a membrane that
can attach to the throat and lead to death by choking. The
disease
is usually spread between people by direct contact or by droplets
through the air, but it can also be
spread by touching contaminated objects such as drinking and eating
utensils, doorknobs or toys. It is more prevalent among
people living in crowded or insanitary conditions.
Before the development of vaccines and treatments, diphtheria was
widespread, mostly affecting children under the age of 15.
Indeed, during the 1930s diphtheria
was
the third leading cause of death in children in England and Wales [14]
– the
outbreak that occurred in Tring in 1891-92 (below) claimed 11 lives. In 1940, diphtheria became the first vaccine of the
bacteriological age to be offered free to British children on a
national scale, since when the disease has become uncommon in the
U.K.:
THE
OUTBREAK OF DIPHTHERIA.
—
Mr. Vaisey
[Town Clerk]
stated that in accordance with a request made by the Local
Government Board, their Medical Officer of Health, Dr. Gruggen,
had given a report on the outbreak of diphtheria at Tring.
This report, which was dated the 31st October, stated that up to
that day there has been twenty-one cases in twelve families, of
which four had proved fatal.
The first case occurred on the 23rd September. Upon making
enquiries he found that the whole family had suffered from sore
throats as far back as the 27th August. With one exception the
whole of the family attacked were under the age of fourteen years
and all the children but one attended to National School at Tring.
As there were no cases from the outlying district he did not order
the school to be closed. He had now reason to believe the
epidemic was subsiding.
He went on to describe the sanitary arrangements of the houses in
which the outbreak had visited. Of the twenty-three houses,
nine had water closets which were not properly flushed, and fourteen
were in a dirty condition. He called the attention of the
Board to the inefficient mode of hand-flushing, and recommended the
use of a siphon tank. He considered that the diphtheria was
propagated from persons by school attendance. He did not think
any suspicion was attached to the milk supply. He recommended
the use of the public water supply in preference to well water,
which should be looked on with suspicion.
In the discussion that ensued, the Chairmen regretted that the
school had not been closed at the commencement of the outbreak. —
Mr. Crouch was in favour of closing the school now, as there was a
fresh case on Sunday last. He mentioned a case where a parent
ought to be prosecuted. Last Sunday week a teacher asked
her class if there were any fresh cases, and a girl got up and said
that her brother had died of diphtheria that very day.
Bucks Herald
7th November 1891
The Clerk read a long report from Dr. Gruggen, Medical
Officer of Health, as to the outbreak of diphtheria at Tring and the
insanitary condition of some places in the town. There had
been 35 cases, and in all 11 deaths — many of the victims, but not
all, having been scholars at the National School. Dr. Gruggen
specified each case, and the state of the sanitation of the houses
in which they were: most of them occurred in November, with a fall
in the barometer and rainy weather after dry. The schools, it
was reported, were closed on December 18th for a three week
vacation.— Mr. Baines said he should be seeing Dr. Gruggen on
Friday, and would inquire as to the desirability of continuing the
vacation. He had two fresh cases of diphtheria to report. —
The Board were of opinion that the holidays might with propriety be
extended. — The Chairman was of opinion that some of the cases to
which Dr. Gruggen called attention were of a serious nature,
and that it was necessary to insist on insanitary premises being put
into a proper condition. The Harrow-yard was mentioned as a
case in point. — The Clerk stated that Dr. Thorne was of opinion
that diphtheria did not arise from insanitation. — Mr. Smith stated
that it was reported, and other members confirmed him, that children
had been allowed by a person to go and kiss the body of a person who
had died from diphtheria, which was regarded as very reprehensible.
Bucks Herald
9th January 1892
Dr. Gruggen continued in office until his death in 1926, which was
announced in the Bucks Herald (30th October):
DEATH OF DR. W.
GRUGGEN.—The death occurred in London on Tuesday week of William
Gruggen, of Durban-road, Watford, one of the best known medical men
in Hertfordshire. About ten day before he died he had a
paralytic seizure while attending a performance at the Regent
Theatre, London, and did not recover. He was 73 years of age,
and leaves a widow and three daughters.
The son of a naval surgeon, Dr. William Gruggen had worked in
Hertfordshire between thirty and forty years. He devoted
himself principally to public health work, and was, at the time of
his death, Medical Officer of Health to a combined sanitary district
that included Watford, Hemel Hempstead, Berkhamsted, Tring, Welwyn,
South Mimms, and Barnet Rural District Councils, and Hemel Hempstead
Borough Council, and Bushey, Berkhamsted and Chorleywood Urban
District Councils. During the war he joined the Herts
Volunteers, and was appointed Battalion Medical Officer.
――――♦――――
MALCOLM GROSS M.B., B.S., D.P.H.
Malcolm Gross was appointed Assistant Medical Officer of Health for
West Suffolk in 1923. Four years later he succeeded the late Dr. Gruggen
becoming
Medical Officer of Health for the Hemel Hempstead Rural District
Council, an area that included Tring.
Both of his predecessors had expressed their concerns about the insanitary
conditions of some of the housing and their surroundings yards in
the town, and over 30
years later Dr. Gross was expressing similar concerns:
Dr. Malcolm
Gross, the medical officer, who could not be present at the Council
meeting, wrote that the Council might remember that in December last
he put forward for consideration a report on housing conditions and
stated that 15 families were in a condition of gross overcrowding.
He also noted the presence of a number of houses of poor
construction and advised that reconstruction was desirable. It
appeared likely that in certain of those cases reconstruction was
unlikely to be carried out and that alternatively closure would be
resorted to, thus making the demand for new housing even greater
than before. It therefore seemed to him that the provision of
further housing accommodation in Tring was a subject which merited
earnest consideration. He always regarded the provision of
satisfactory housing as the foundation upon which so many other
health measures are based and without which much of their value was
dissipated.
Bucks Herald
8th November 1929
Diphtheria also remained high on the Medical Officer’s agenda, this
from a Town Council meeting held in 1933:
DIPHTHERIA IN
TRING AREA.―The Sanitary Inspector reported that there had been
three cases of diphtheria, two of tuberculosis and one of pneumonia.
Dr. Gross said that it was a fact that there had been trouble
with diphtheria during the past two months, but he did not think
they would have any more trouble. It was very difficult to
trace the original source. Of course, there had been cases
round about Tring, and there had only been ten cases during the
year. Really there had been no definite outbreak, which made
it all the more difficult to trace, although they had traced one or
two cases. Also they had found that one or two children were
carriers.
Bucks Herald,
6th January 1933
In an age before
the state paid for vaccination it fell to parents to find the money
to have their children treated. Here Dr. Gross proposes a
scheme whereby the Council would pay for diphtheria vaccination in
eligible cases:
The Chairman
[of Tring
Town Council]
mentioned that the Medical Officer had submitted his scheme for
diphtheria immunisation, which would be available for children of 1
to 14 years of age, of parents in the Council’s area who could not
afford to pay for the treatment privately. The Council would provide
the materials and pay the medical practitioners a fee of 2 shillings for
each child treated.
Dr Malcolm Gross said he did not anticipate that a large number
would ask for treatment, but he would like the Council to be able to
say that the treatment was available for the children of parents who
could not afford the treatment privately. The scheme was adopted in
other parts of the county, and in other counties, and very
extensively in the big cities. On the proposition of Councillor
Wright, seconded by Councillor Goddard, the scheme was adopted for
six months.
Bucks
Herald 7th February 1936
Dr. Gross was born in Wandsworth on the 2nd August
1890 and died in Hemel Hampstead in 1970.
――――♦――――
LICENSED TO DRILL:
THE EVOLUTION OF DENTAL CARE
Among the ‘Medical Men of Tring’ are those who practise dentistry.
This is the specialist branch of medicine that is focused on the
treatment of dental/oral disease, the correction of dental
irregularities and the treatment of dental/facial injuries.
Those who practise this branch of medicine are called “dentists”.
Today it’s a criminal offence for a person who is not a registered
dentist to practise dentistry; however, this restriction is
comparatively recent. Although approved dental training and
qualification did exist beforehand it was not mandatory, and into
the early 20th Century anyone could practise dentistry. The result
was that in addition to capable and conscientious
practitioners were many
others who were unskilled and uneducated. Indeed, until the
passage of the Dentists Act of 1921, dentistry in itself could not
be described as a
profession.

The Quack Tooth Puller by
Theodoor Rombouts (c.1620 and 1625).
Although evidence of the practise of dentistry extends back to
prehistoric times, in Britain it was not until the 17th Century that
there was any written guidance on the subject.
‘The Operator For The Teeth’, published in 1685 by Charles
Allen, was the first dental textbook to be written in English.
Among other things Allen explained that diseased gums can be
prevented and cured by “regular removal of the scales” and that
teeth are composed of two tissues. He also used the term
enamel, apparently for the first time. To quote from his
text:
“In
analysing the tooth, its substance is not found to be uniform
everywhere, but manifestly distinguishable into two different sorts
of make: one of them being harder, whiter and of finer texture; and
the other softer, more obscure and of a coarser composition.
The exposed part of the tooth consists also of two different parts.
To wit, its stony cover or case, and its inward substance; the first
is as it were a hard periosteum, that invests the head of the tooth
on all sides, lying on it much after the same manner that Enamel
does upon Gold, or any other thing.
This natural Enamel which I call the gloss of the tooth is of a far
harder, whiter, more dense and lucid nature than the inward
substance lying under it.”
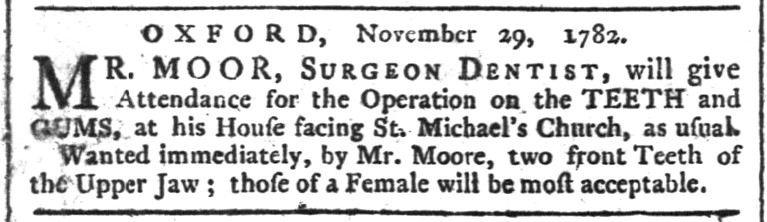
30th November 1782, The
Oxford Journal.
Allen also gives an unedifying description of the procedure to be
followed in transplanting teeth, using animals as donors:
“First I
would choose an animal whose teeth should come nearest to those of
the patient; as a Dog, a Sheep, a Goat, or a Baboon etc. and having
tied his legs together, I would fasten his head in some convenient
place, so that he might not stir in the least, and by some proper
means keep his mouth open, as long as I should have occasion: that
done, I would open the gums around the tooth to be taken out of his
head, not only to the very jaw-bone, but as far between the said
bone and the tooth, as the finest Instrument could go; leaving a
very little portion of the gums about it, and then having used the
same circumspection, in dividing the Patients tooth from the gums,
and the Jaw-bone, I would draw it forth, and put immediately in its
place that of the Brute, fastening it very well and straight between
the other teeth.”
The establishment of Allen’s textbook created a scientific network
of knowledge for those interested in a dental career, but without
the legal requirement to obtain a recognised dental qualification
– and a body to register those who did – the work of untrained and
unqualified practitioners proliferated. The following report
is, perhaps, a
more extreme example of quack dentistry:
“BOW
STREET.―An Italian image-maker and his wife, named Ambrogi, residing
in Leather Lane, Holborn, came to complain of the unskilful conduct
of a dentist under the following circumstances:―
The complainant stated that about five weeks ago his brother,
Constant Ambrogi, being severely tortured by the tooth-ache, went to
a dentist, residing in Longacre, for the purpose of having the tooth
extracted. The dentist, after putting him to great torture in
attempting to extract the tooth, broke his jaw, and actually carried
away a portion of the flesh with his instrument.
The young man returned home, and remained in the greatest agony
until the following evening, when he was advised to go to Dr Owen,
who resides in Holborn. That gentleman told him that his jaw
was broken, and asked him the name of the dentist who had performed
the operation; and having been told who he was, and where he lived,
he drew a splinter from the jaw of the deceased, which put him to
great pain, and giving him some castor oil told him to go home an
keep himself quiet, and he would soon get well. The deceased
attempted to swallow the castor oil, but it would not remain in his
stomach, and after lingering some days in the greatest possible
torture, the jaw mortified and death ensued.”
Bucks Gazette -
Saturday 12 January 1833.
Dental procedures were often performed by travelling dentists among
whom – judging by their newspaper advertisements – were a high
proportion of quacks. One such itinerant practitioner was
William Lukyn, who for a number of years advertised his services in
the Aylesbury press as both a maker of artificial teeth and a
practitioner in the “extraction, plugging and any other operation
on a tooth”.
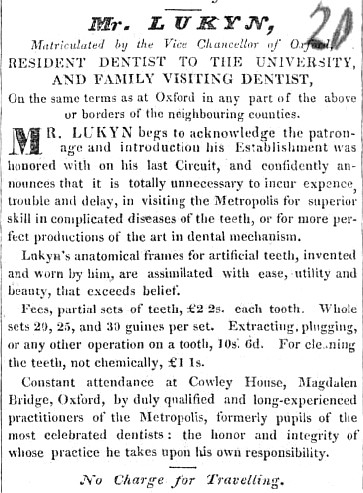 |
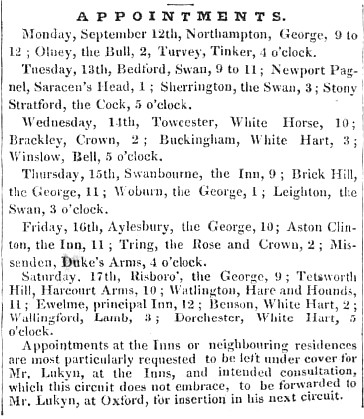 |
|
Bucks
Herald, 10th September 1836. |
Lukyn advertised his “circuit” in local newspapers, informing
readers at which public houses he could be consulted and when; at
Tring he appears to have favoured the Rose & Crown. To give
readers the impression that he was a man of learning his
advertisements sometimes contained a sprinkling of Latin, while his
claim to have “Matriculated by the Vice Chancellor of Oxford,
RESIDENT DENTIST TO THE UNIVERSITY” gave further substance to that
impression. But his reference to the University and his
alleged university training eventually came to the attention of the
authorities who expressed their disapproval in a strongly worded
notice published in the Bucks Herald.
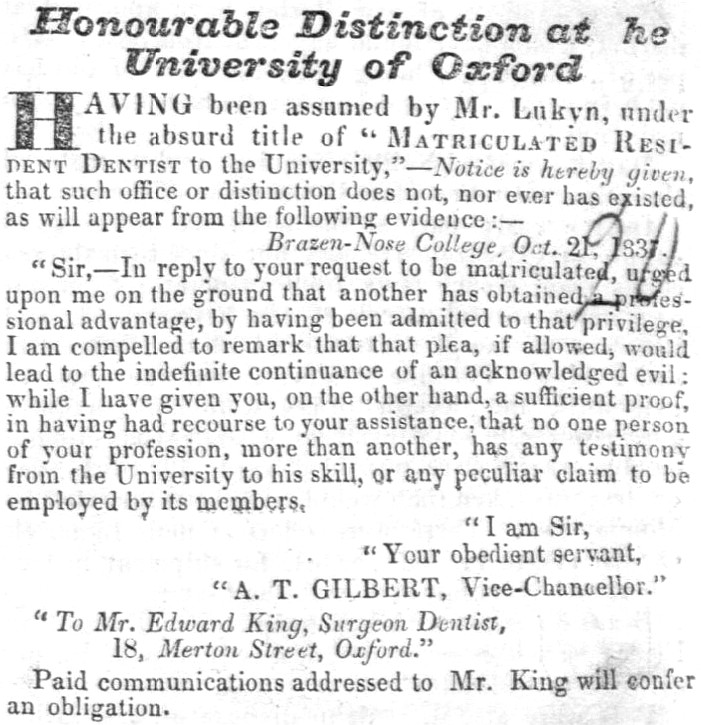 |
|
Bucks
Herald, 8th September 1838. |
The Royal College of Surgeons in London had already posted a similar
notice disowning Lukyn in the Bucks Herald:
“Sir, ― In
reply to your inquiry of the 27th instant, I have to inform you that
Mr. William Lukyn is not a Member of this College.
I am, Sir
Your most obedient servant,
Edward Balfour, Secretary.”
Despite this adverse publicity Lukyn appears to have remained in
business for some years thereafter, the last mention of him being a
press notice inserted by the proprietor of the Bucks Herald
requesting settlement of a debt, presumably for Lukyn’s advertising:
“We have
sent our bill to Mr. Lukyn, dentist, Oxford, and receive no
attention. A subscriber, at Leamington, acquaints us that the
Oxford Matriculate is at Leamington, where he will read this notice
of his neglect, which we shall be happy to amend comme il faut.”
Bucks Gazette,
17th October 1846.
The late 1850s marked the beginning of the transition of dentistry
in England from an art of the sort practiced by William Lukyn to the
profession we recognise today. The Medical Act of 1858
permitted the Royal College of Surgeons of England (RCS England) [17]
to grant licenses in dental surgery. This section of the Act
applies to dentistry:
“XLVIII:
Her Majesty may grant Power to College of Surgeons to institute
Examinations, &c. for Dentists. It shall, notwithstanding
anything herein contained, be lawful for Her Majesty, by Charter, to
grant to the Royal College of Surgeons of England Power to institute
and hold Examinations for the Purpose of testing the Fitness of
Persons to practise as Dentists who may be desirous of being so
examined, and to grant Certificates of such Fitness.”
In the United Kingdom, the first dental schools – the London School
of Dental Surgery and the Metropolitan School of Dental Science,
both in London – opened in 1859, while 1860 saw the
first licenses in dental surgery (L.D.S.) awarded by the RCS. [18]
The Medical Act of 1858 was designed specifically to regulate the
qualifications of practitioners in medicine and surgery, and it made
no other mention of dentistry than in section XLVIII referred to
above. Perhaps this is indicative of how little importance was
then attributed to dental care, which later in the century gave rise
to alarming statistics: of the British Army’s recruits for the Boer
War, of 208,300, there were 6,942 hospital admissions owing to
dental causes of which one third had to be sent home as unfit to
serve.
|
 |
|
Lilian Lindsay
CBE LLD MDS HDD FDS (Eng&Edin) FSA (1871–1960).
The
first woman to gain a British dental qualification and a
leading member of the profession |
The Dentists Act 1878 was the first legislation to regulate
dentistry by limiting use of the title “dentist” and “dental
surgeon” to registered practitioners. Under the Act the four
surgical Colleges in the UK and Ireland [19]
received authorisation to establish a qualification through
examination that would lead to registration on the ‘Dentist
Register’, at that time held by the General Medical Council (now by
the General Dental Council). However, not only was registration
voluntary, but registered dentists were encouraged not to
advertise their services as this was considered to bring the
profession into disrepute. Unregistered dentists could remain
in practice subject to the “dentist”/“dental surgeon” stipulation,
and could also advertise their services profusely to attract
patients.
Thus, for some
decades the fledgling profession remained full of untrained and
unqualified practitioners:
“. . . .
there is nothing to stop Tom, Dick or Harry setting up as a dental
surgeon. London was overrun with ‘quacks,’ who had all sorts
of wonderful ‘degrees’ from American correspondence colleges.
Quite a lot of dental mechanics, after a few years employment in the
manufacture of plates, set up on their own every year as ‘dentists’
fully qualified to deal with every disease of the teeth.
The Committee who had been appointed to inquire into the subject had
reached the root of the matter when they reported that at the
present, legal decision has brought within the lawful occupation of
any man the practise of dentistry provided he does not use the
description of ‘dentist’ or ‘dental practitioner’ or any name or
title, etc. implying that he is registered under the Dentists Act.”
Pall Mall Gazette,
24th November, 1919.
This situation had to await the Dentists Act of 1921, which made it
mandatory for newly qualified dentists to register with the
Dental Board of the UK. Further legislation in 1956 replaced
the Dental Board with the General Dental Council (GDC) with the aim
of making the dental profession a self-governing profession.
The GDC was given the role of promoting high standards of
professional education and professional conduct among dentists in
addition to controlling such matters as dental education and
examinations, and determining disciplinary cases.
Later legislation (1984 and 1986) provided for the enrolment and
regulation of dental therapists and dental hygienists, while an
Amendment Order in 2005 introduced compulsory indemnity cover and
allowed the GDC to regulate the whole dental team, including dental
nurses and dental technicians, and to take action in cases of poor
professional performance.
One wonders what the GDC would make of Mr Lukyn!
DENTISTRY IN TRING
It is difficult to say anything about the practise of dentistry in
the town in a bygone age, for unlike the town’s doctors,
dentists were not, as a general rule, confronted with cases
that were likely to attract the attention of the press. As the
first part of this paper illustrates, reports of serious infectious
disease, serious injury, or any medical matters resulting in a court
hearing did occasionally find their way into the local newspapers,
thereby provided some insight into the work of the town’s doctors;
but of dentistry, other than newspapers advertising their services, there is
nothing.
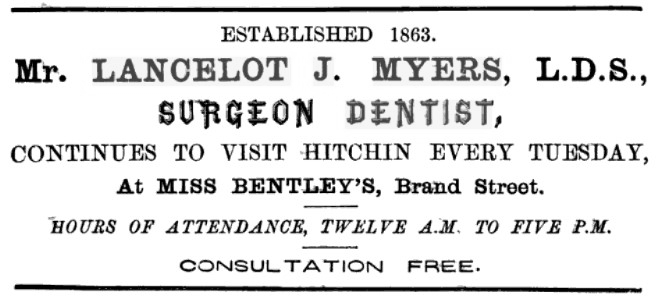
Myers’
entry into dental practise 1863.
(Handbook to
Hitchin, 1875)
In 1863 a notice appeared in the November edition of The
Lancet announcing that Lancelot J. Myers (among others) “had
received their diplomas in Dental Surgery, at a meeting of the Board
of the Royal College of Surgeons of England” making Myers one of
the earliest dentists to obtain this professional qualification.
Two years later the Hertfordshire
Express announced that Myers was working - presumably in
partnership - with Henry Faulkner. Faulkner described himself
as a “Surgeon Dentist” but his professional qualifications to
perform that role - i.e. “Formerly Assistant to the Dentist by
Appointment to Her Majesty’s Household” - look distinctly
dubious whereas Myers was suitably qualified. Later advertisements show Myers - by then practising
on his own - making weekly visits to Tring, although no information
is given as to where he might be consulted. Presumably patrons
of the Tring’s public houses were well aware. These
advertisements continued until 1899.
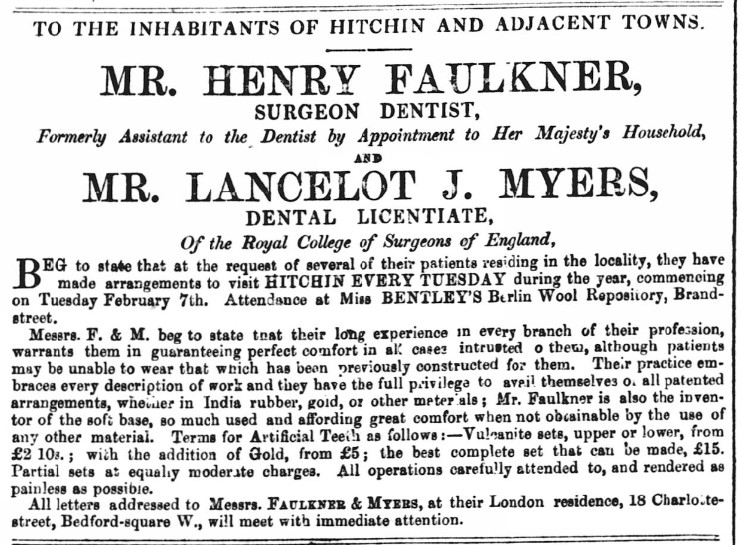
Herts Express, 28th January 1865.
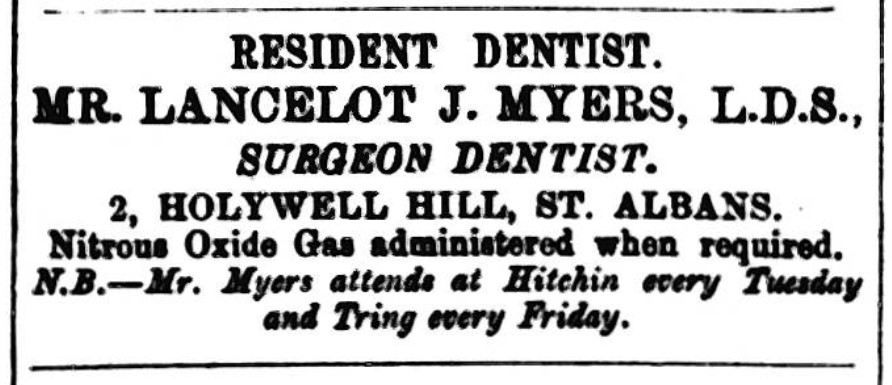
Herts Advertiser, 23rd February 1884.
Newspaper advertisements suggest that Myers continued to
practise until September 1906, although they show that by then
visits to Tring were no longer in his itinerary.
Another itinerant dentist whose occasional visits to Tring
appear to have overlapped with those of Myers, was George Mather
Horsey. Horsey stated his professional qualification as
being “a Doctor of Dental Surgery”, which when
taken with his claim to perform such feats of dental surgery as
the “full restoration of facial features and youthful
appearance” makes one wonder on first sight whether he was a
graduate of the same school of dentistry as
William Lukyn. But in his later more modest adverts, his
claim to hold a License in Dental Surgery from the Royal College
of Surgeons suggests that at some point in his career he
successfully underwent professional training in dentistry.
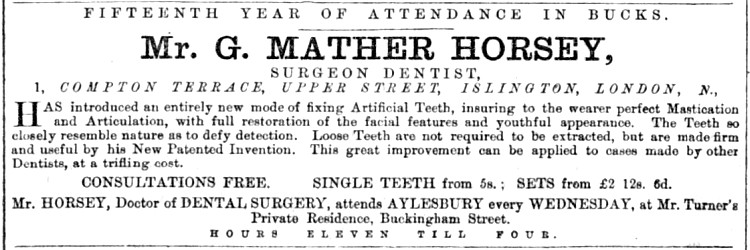
Bucks Advertiser,25th July 1867.
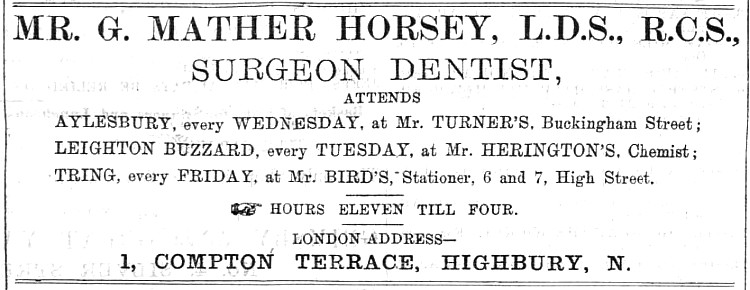
Bucks Herald, 26th July 1884.
According to
his advertisement, when in Tring Horsey set up shop at the
premises of the town’s printer and stationer, Ebenezer Bird,
whose shop, long demolished, stood opposite the
Forge Car Park in
Tring High
Street. In later years his advertisements suggest that
Horsey’s practice was confined to Aylesbury where he seems to
have prospered, for when he he died in November 1925 the gross
value of his estate was given as £32,203, or approximately
£2,505,000 at 2023 valuation.

The premises of E. C.
Bird, printer and stationer, are on the left of the picture.
Within the date range in which I’m working (1780-1939) the trade
directories for Tring that I have access to, [20]
list only three dentists in the town:
|
Kelly 1914 and 1926 |
Alfred John Higson LDS RCS (Eng) |
Mondays 2-4pm, Western Rd. |
|
Kelly 1926 |
George S. Dingley LDS RCS (Eng) |
Bayley, Western Rd. |
|
Kelly 1937 |
Mervyn Snipper LDS RCS (Eng) |
Bayley, Western Rd. |
Of the above Mervyn Snipper is known to have left the area for a
practice in London in 1938.
At the time of writing there are four dental practices in Tring.
――――♦――――
|
